HHV-6/7 DNA was found in the plasma of 19.6% of epilepsy patients compared to none of the controls. Protein expression, indicating active infection, was found in 53% of the HHV-6/7 positive patients. Roseolovirus sequences were also found in the whole blood of 87% of epilepsy patients vs. 55% of controls.
The study, published in Brain Sciences by investigators from Riga Stradins University in Latvia, demonstrated that patients with epilepsy not only display a higher of frequency of roseolovirus (HHV-6A, HHV-6B, and HHV-7) infection than control groups, they have higher viral loads, and increased viral gene expression, HHV-7 positive patients exhibited increased levels of the proinflammatory cytokine TFN-alpha. Epileptic patients also displayed expression of the HHV-6 U89/90 gene, which regulates viral latency and reactivation.
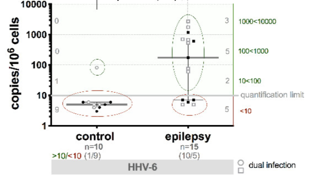
Viral load in whole blood was significantly higher in epilepsy patients than in controls. 10/15 patients with epilepsy and only 1 of the control group individuals had a viral load of >10 copies/106 cells.
Inflammation is known to be involved in epilepsy and meta-analyses have shown elevated levels of TNF-alpha in epileptic patients. The authors point out that HHV-6 & 7 can both modulate cytokine secretion and modulate the chemokine system, and that viral infections are a risk factor for epilepsy. The authors conclude that the combination of active infections, expression of the HHV-6 U89/90 gene, and the levels of TNF-alpha in HHV-7 positive patients provide a possible mechanistic explanation for roseoloviruses as etiologic pathogens in a subset of epilepsy patients.
A Japanese study found that HHV-6B plays a pathogenic role in epilepsy by enhancing gene expression that induces neuroinflammation and sclerosis in the temporal lobe. They found that neuroinflammation-enhancing monocyte chemotactic protein-1 (MCP-1) was significantly increased in HHV-6 positive vs. negative brain samples from epilepsy patients (Kawamura 2015). Active HHV-6B infections are found in 32% of infants with febrile status epilepticus (Epstein 2012), and approximately 30% of these infants go on to develop mesial temporal lobe epilepsy (MTLE). One study found HHV-6B DNA in 69% of resections from MTLE patients, compared to 0% of controls (Fotheringham 2007).
Epilepsy is one of the most common neurological disorders in the world, affecting approximately 1% of the population. Despite the wide variety of medications on the market, roughly 30% of patients have not found a treatment regimen that controls their seizures. Identifying etiologic pathogens would greatly advance the available care for people suffering from epilepsy, and these results lay a crucial groundwork for further research in controlling this debilitating disease.
Read the full paper: Rasa-Dzelzkaleja 2020