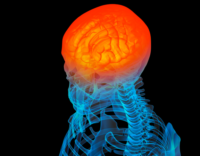
A fifth case of limbic encephalitis associated with GAD antibodies and HHV-6 infection has been reported, this time in an immunocompetent woman with chromosomally integrated HHV-6, epilepsy, and psychosis. The patient’s condition improved (with a drop in GAD antibody titers and stabilization of psychotic symptoms) in response to three weeks of antiviral therapy but relapsed when antiviral therapy was withdrawn.

Pitt Niehusmann, MD.
Consultant, University Hospital Oslo
Norway
Previously, the same neuropathology group in Germany reported two GAD-antibody-positive limbic encephalitis patients with HHV-6 DNA detected in surgically removed hippocampal tissue (Niehusmann 2010). Another publication reported two patients who had HHV-6-associated limbic encephalitis, autoimmune thyroid disease, and elevated antibodies to GAD (Mata 2008).
GAD antibodies occur in a number of neurological disorders, and when the antibodies are extremely high, they can cause Stiff Person Syndrome. High level GAD antibodies define a relevant group of patients with chronic, nonremitting, and nonparaneoplastic limbic encephalitis (Malter 2010). At low levels, these antibodies are a predictive factor for type 1 diabetes.
The authors note that antibodies against NMDAR, the surface protein N-methyl-D-aspartate receptor, have been identified as a cause of encephalopathy post HSV-1 encephalitis, and speculate that HHV-6 may trigger a similar cascade. They recommend further study to determine the frequency of simultaneous active HHV-6 infection and GAD65 antibodies. Of interest, a 1998 report identified GAD65 antibody stimulation in response to the HHV-6 U2 gene, via mimicry (Bach 1998).

Professor Dr. Albert Becker, MD
Professor for Molecular Neuropathology
Translational Epilepsy Research
University of Bonn, Germany
HHV-6 reactivation has been linked to many of the conditions associated with GAD antibodies. For example, HHV-6 reactivation has been found in cases of fulminant type 1 diabetes after drug induced hypersensitivity syndrome (DIHS). In one series, HHV-6 reactivation was linked to 11 cases of fulminant type 1 diabetes (Onuma 2012). Two other cases of drug hypersensitivity and type 1 diabetes were reported by Taiwanese investigators in association with DRESS (Chiou 2006).
Immunohistochemistry of brain tissue from this case showed T-lymphocytic infiltrates, a moderate activation of microglia, and moderate reactive astrogliosis. Anti-neuronal antibodies binding to pyramidal cells of the hippocampus and cerebellar Purkinje cells within the serum and CSF were identified using an indirect immunohistochemistry approach.
The study was led by neuropathologist Pitt Niehusmann, MD from University Hospital Oslo, Norway and Albert Becker, MD from the Translational Epilepsy Research Section at the University of Bonn, Germany.
For more information, read the full paper (Niehusmann 2016).