Evidence linking neuroinflammation to epilepsy, and viral infections, particularly from HHV-6, are a plausible cause of that neuroinflammation (Bartolini et al. 2019). Mechanisms involving chronic inflammatory processes, leading to neuronal excitability or increased blood-brain permeability have been proposed.
A group led by Steven Jacobson of the NINDS studied 46 children within 24 hours of seizures and 43 healthy controls, analyzing cytokine levels in plasma and saliva as well as performing viral load measurements of HHV-6 and EBV DNA using droplet digital PCR. Seizure patients exhibited significantly higher plasma cytokine levels, particularly of CCL11, CCL26, IL-10, IL-6, IL-8, and MIP-1B (Figure 1). Salivary cytokine levels did not correlate with plasma levels.
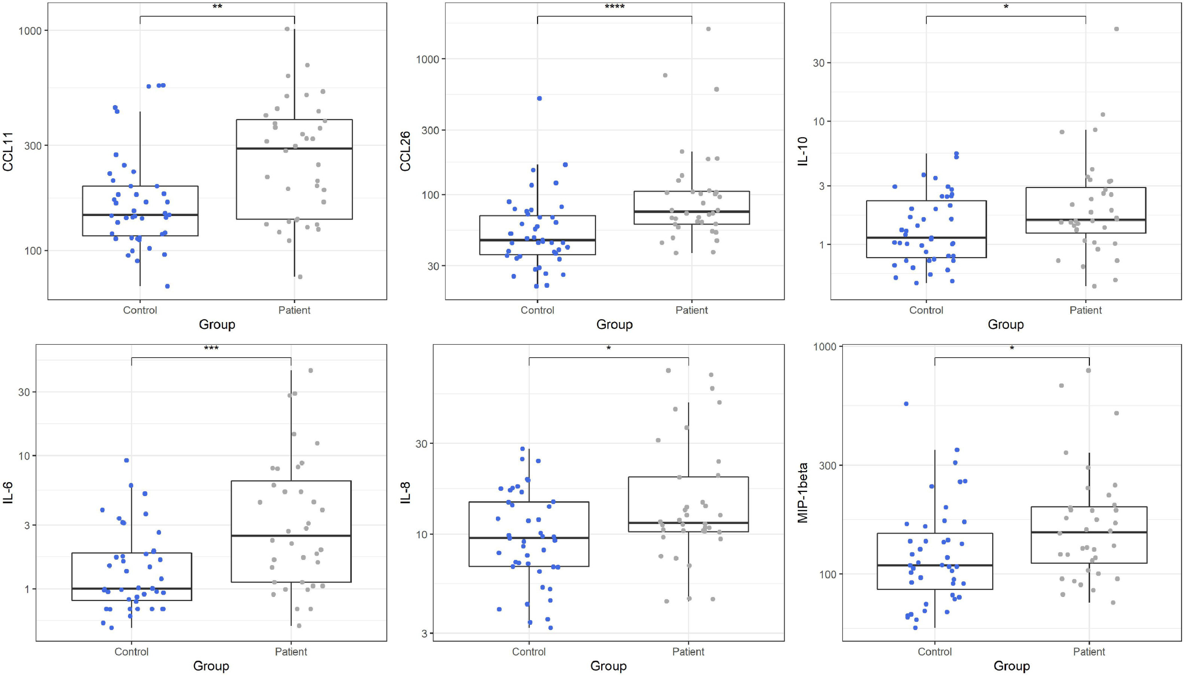
Figure 1: Cytokine levels in plasma for cases vs. controls
DNA from HHV-6 and EBV was not detected more frequently in cases than in controls. Larger past studies have found active infection in 13% of infants with febrile seizures and 32% of those with febrile status epilepticus (Hall 2003, Epstein 2012). This study included only 6 children with febrile or complex seizures; the rest were new chronic or new onset epilepsy patients.
The lead author demonstrated previously that there can be extremely high viral loads in the brain tissue, with blood levels nearly undetectable (Fotheringham 2007). Indeed, the most persuasive past research linking HHV-6B to epilepsy has evaluated tissue from the brain, particularly the mesial temporal lobe, or cerebrospinal fluid, rather than the plasma; no such tissue was examined in this study. One small group of seizure patients had atypical activation of IFNy/CXCL10/IL-10 pathway, suggesting a possible link with a viral infection.
In summary, this study found evidence linking systemic markers of inflammation to some types of epilepsy.
Read the full article: Bartolini et al 2021

