Australian investigators studied 143 young children with febrile seizures for signs of viral infection and found that HHV-6 was the fifth most common virus after rhinovirus (22%), enterovirus (20%), adenovirus (21%) and influenza (13%). Overall, a virus was found in 71% of cases. Complex seizures were associated with HHV-6 (42%) or influenza (41%).
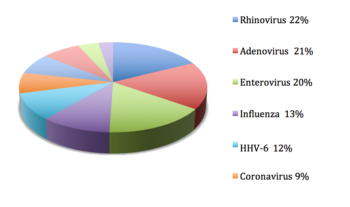
Viral infections in Australian infants hospitalized for febrile seizures. Source: Francis 2016
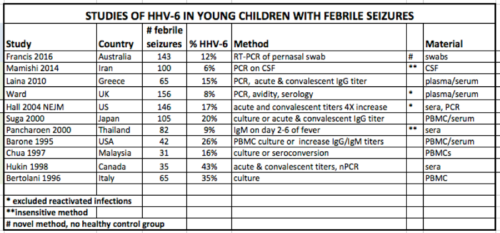
Previous studies have shown that HHV-6 and HHV-7 are both associated with febrile seizures. The largest study of 146 infants with febrile seizures reported that 17% had seizures due to HHV-6 primary infections (Hall 1994). A recent review of 8 other studies on HHV-6 in febrile seizures found a similar rate of 17% (Mohammadpour Touserkani 2016).
The prevalence in past studies varies according to methods used and whether or not reactivated infections are included. An NIH funded study of 199 infants with febrile status epilepticus (FSE) determined that 32% had an active HHV-6B infection and 7.1% had active HHV-7. This study did not exclude children with reactivated infection, and those cases accounted for 30% of the cases of HHV-6 viremia. Active infection was determined by testing for mRNA in PBMCs (Epstein 2012).
Source: HHV-6 Foundation
On the other hand, in the UK, investigators excluded patients with reactivated infections by counting only patients with low avidity (an indication of a recent primary infection). They found primary infection of both HHV-6 and HHV-7 in febrile children with convulsions each at a rate of approximately 8% (Ward 2005). As with the Australian study, the subset with HHV-6 or HHV-7 in the UK tended to have more severe cases; 18 of the 25 (72%) young children with HHV-6 or HHV-7 had status epilepticus.
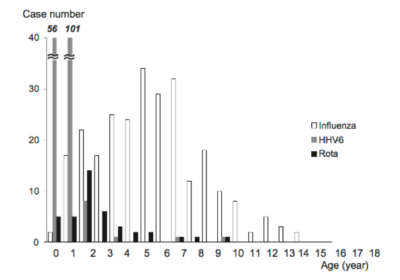
Age distribution of viruses found in children with encephalopathy in Japan (Source: Hoshino 2011).
In Japan, a nation-wide survey of acute encephalopathy in 983 cases found that HHV-6 was the second most common pathogen implicated in the condition, and was by far the most common cause of encephalopathy in infants under the age of two with a peak at 9 months. In older children, influenza was the most common pathogen (median age 6 years). Rotavirus and RSV were the third and fourth most common pathogens (Hoshino 2012).
Impact of vaccination on risk of febrile seizures
The Australian study was consistent with past reports showing a significant increase in seizure risk following a live vaccine; 11% of the febrile seizures occurred within two weeks of a vaccination, almost all of them after the MMR (measles, mumps, rubella). Other studies have shown an increased risk for seizures after the MMR, including a large study of 679,942 children that reported a 2.8 fold increased risk of febrile seizure in the 8-12 days after live MMR vaccination (Barlow 2001). Furthermore, adding live varicella virus (MMR-V) to the vaccination increases the risk of febrile seizure 8-12 days after the vaccination by two fold over the risk of the MMR alone (Klein 2015). Of note, the administration of the MMR at 12 months coincides with the peak period of HHV-6 primary infections at 6-11 months (Hall 1994), raising the question of whether the live vaccine might be able to reactivate HHV-6 after a recent primary infection.
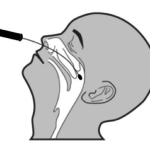
The Australian group use a pernasal swab to look for infections in infants with febrile seizures.
Weaknesses of the study include the fact that pernasal swabs were used instead of plasma DNA or blood mRNA, and the fact that there was no control group of healthy children. Also, the PCR testing was not quantitative, so it was not possible to differentiate between a high level infection and a low level of virus that might be found in a healthy control. The authors note that low levels of adenovirus, rhinovirus and enterovirus but not influenza can be found in the nasopharyngeal cavity of healthy control children (Wiersema 2011). One small study found no evidence of HHV-6 in the nasopharyngeal cavity of healthy adults (Kositanont 1993), but the prevalence in children is unknown.
For more information, read the full paper: Francis 2016.