NINDS investigators studied fresh resected brain tissue and found 29 of 54 positive for HHV-6 DNA. Previous studies using formalin fixed and paraffin embedded samples have yielded much lower rates of positivity.
Many studies have found evidence that HHV-6 infection of the brain is one possible trigger for mesial temporal sclerosis (MTS) and mesial temporal lobe epilepsy (MTLE). The strongest evidence comes from studies looking for viral nucleic acid and antigens in resected brain tissue from patients treated surgically to eradicate epileptogenic foci. However, past studies have found very different rates of virus in such tissue, due to different techniques and type of tissue utilized (eg. frozen, fresh or formalin-fixed paraffin embedded samples prone to degradation over time).
A study led by Steve Jacobson and William Theodore at the National Institute of Neurological Disorders and Stroke, used fresh tissue samples immediately processed after resection to compare detection of HHV-6 in patients with MTS to other epilepsy etiologies. 87 patients who had surgery between 2001 and 2017 were included. Viral nucleic acid detection was done with both quantitative real-time PCR (RT-PCR) and digital-droplet PCR (DD-PCR) specific for HHV-6A and HHV-6B, and with a sensitivity of 40 viral copies/milliliter. Surgery samples tested included those with MTS (n=54), focal cortical dysplasia (FCD) (n=23), and patients whose epileptogenic foci were associated with encephalitis (n=3). Samples from those with excised brain tumors (n=4) and vascular lesions (n=3) were also studied.
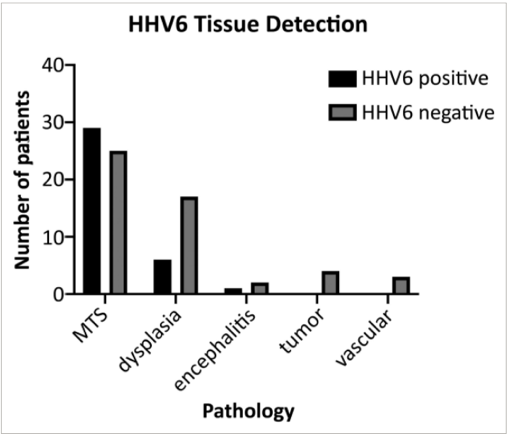 Patients with MTS were significantly more likely to have HHV-6 detected in these surgical resections than those with other pathologies. HHV-6 was detected in 29/54 (54%) of patients with MTS, 6/23 (26%) of patients with FCD, and in one patient with Rasmussen’s encephalitis (P<0.02). Febrile seizure history was not associated with HHV-6 detection. In MTS patients, there was also no difference in onset age between HHV-6 positive and negative patients. Of the HHV-6-positive cases, 26 were positive for HHV-6B, 5 positive for HHV-6A, and 6 were positive for both viruses. Positron emission tomography (PET) revealed a trend toward enhanced microglial inflammation in the seizure foci of patients positive for HHV-6.
Patients with MTS were significantly more likely to have HHV-6 detected in these surgical resections than those with other pathologies. HHV-6 was detected in 29/54 (54%) of patients with MTS, 6/23 (26%) of patients with FCD, and in one patient with Rasmussen’s encephalitis (P<0.02). Febrile seizure history was not associated with HHV-6 detection. In MTS patients, there was also no difference in onset age between HHV-6 positive and negative patients. Of the HHV-6-positive cases, 26 were positive for HHV-6B, 5 positive for HHV-6A, and 6 were positive for both viruses. Positron emission tomography (PET) revealed a trend toward enhanced microglial inflammation in the seizure foci of patients positive for HHV-6.
In this study, a higher proportion of samples positive for HHV-6 was found when compared to other literature. The most likely explanation for this is that this study examined fresh resected tissue with highly sensitive technologies.
These results support a potential role of HHV-6 in the etiology of MTLE/MTS. As summarized by the authors, HHV-6 could promote epileptogenesis through several potential mechanisms.
Read the full article: Theodore et al. 2021