HHV-6 IgM antibodies were higher in pregnant MS patients than in healthy controls. Women with elevated HHV-6 IgM titers were more likely to relapse postpartum.
Over the past 60 years, multiple sclerosis (MS) has been linked to many possible infectious triggers. Many of these putative triggers have not withstood the test of time. In the past 20 years, however, three viruses have increasingly been linked to MS: Epstein-Barr virus, human herpesvirus 6A and MS-associated retrovirus (MSRV) (Mentis 2017; Komaroff 2021).
During pregnancy, the rate of recurrent attacks of MS seems to drop, only to increase again in the postpartum period, for unknown reasons (Hellwig 2012). Perez-Perez et al. (2021) of the Instituto de Investigación Sanitaria del Hospital Clínico San Carlos measured antibody titers for EBV, HHV-6A/B, and also measured the expression of mRNAs for MSRV envelope proteins in pregnant MS patients (P-MS) and pregnant healthy controls (P-HC), both during pregnancy and in the postpartum period.
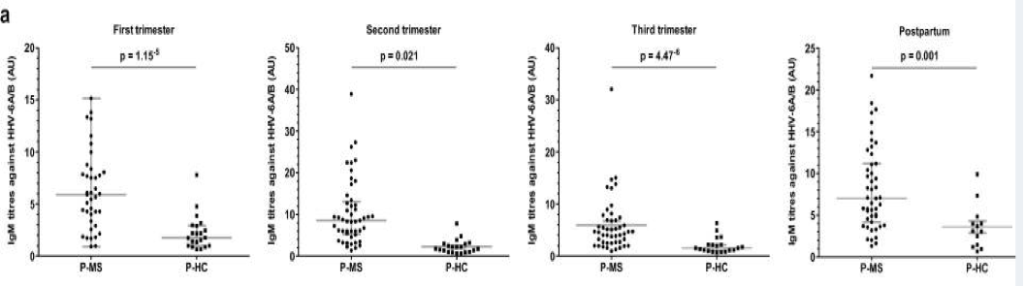
a) IgM antibody titers against HHV-6A/B in various trimesters/postpartum period for P-MS/P-HC groups
IgM antibody titers against HHV-6A/B were significantly higher in the P-MS patients than in the P-HC, in every trimester and in the postpartum period. Within the P-MS group, anti-HHV-6A/B antibody titers were also somewhat higher in the 1st trimester for those who subsequently relapsed in the postpartum period than it was in those who did not relapse postpartum. In contrast to the results with IgM antibodies, levels of IgG antibodies against EBV or HHV-6A/B were not different between P-MS and P-HC.
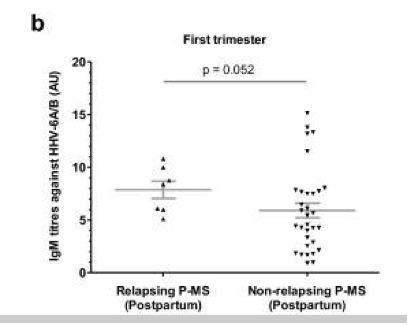
b) IgM antibody titers against HHV-6A/B in the first trimester for those in the P-MS group who did and did not relapse in the postpartum period.
The expression of MSRV envelope protein mRNA in the 1st trimester was also more prevalent in those MS patients who experienced relapses during gestation.
These findings are consistent with previous reports linking active HHV-6 infection with MS, particularly with exacerbations of MS (Ortega-Madueno 2014). The evidence linking the expression of mRNAs from MSRV to MS is not as strong, but also consistent with some previous studies. Moreover, it is plausible that EBV, HHV-6 and MSRV might interact synergistically in generating relapses of MS. Identifying biomarkers in the 1st trimester of pregnancy that indicate an individual with MS who is at risk for a relapse in the postpartum period might help focus people most able to benefit from treatments to prevent relapses, although this remains to be demonstrated.
Read the full article: Perez-Perez 2021

