Sera drawn before vs. after onset of MS find seropositivity for HHV-6A more likely in MS.
There is considerable evidence that infection with Epstein-Barr virus (EBV) is a necessary condition for the development of MS. The best study found that primary EBV infection occurred, on average, about 7.5 years before the onset of MS (Bjornevik 2022). Evidence consistent with molecular mimicry between an EBV protein and a molecule expressed in MS plaques has suggested a mechanistic link (Lanz 2022). Also, following EBV seroconversion, levels of a marker of neuronal injury—serum neurofilament light chain (sNfL)—started to rise in those people who, following primary EBV infection, went on to develop MS.
Nevertheless, since most humans are infected with EBV but do not have MS, cofactors likely also are required for MS to develop. Furthermore, molecular mimicry in animal models usually produces disease relatively quickly—and this is not consistent with the 7.5 years between first exposure to the viral antigen and the clinical presentation of the disease. This, too, suggests cofactors may be involved.
HHV-6A also has been associated with MS, and some evidence suggests that infection with both viruses may have a synergistic effect in triggering MS (Engdahl 2019; Bistrom 2021). A Swedish team merged an MS registry with multiple biobanks to study evidence of infection with multiple human herpesviruses before and after the development of relapsing-remitting MS. For each case, a control subject without MS—matched by gender, birth date and blood sampling date—was identified. There were 670 matched case-control pairs; their median age at sampling was 24.7 years. Serological studies for HHV-1 through HHV-7 were performed, and measurements of sNfL levels obtained. The investigators used a bead-based multiplex assay that measured the seroresponse against a truncated immediate-early protein 1 from HHV-6A (IE1A), as well as against EBV EBNA-1. A previous study showed that the IE protein of HHV-6A, but not the late protein for HHV-6A or any HHV-6B protein, was associated with MS (Bistrom 2021).
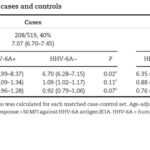
HHV-6A seropositivity was greater in cases (40%) than in controls (25%, P<0.001), as summarized in Table 1, below. As would be expected, levels of sNfL were greater in cases than in controls, particularly in those who were HHV-6A seropositive and younger than 24.7 years. Levels of sNfL were higher in cases who were seropositive for both EBV and HHV-6A than in those who were seropositive only for EBV, particularly in patients younger than 25 years of age. There was no serological association of MS with the other human herpesviruses, including HHV-6B and HHV-7. Antibody levels to HHV-6A started rising before levels of sNfL began to rise, demonstrating that HHV-6A reactivation preceded neuronal injury, demyelination and the first symptoms of MS.
While this study provides additional evidence suggesting that infection with HHV-6A may, along with EBV, be involved in triggering relapsing-remitting MS in at least some cases, there are some caveats. First, many healthy controls also were seropositive for HHV-6A. Second, many controls also revealed some evidence of neuronal injury, raising questions about the specificity of the sNfL biomarker for neuronal injury.
This study does not provide evidence that HHV-6A is a required for the triggering of MS, but is consistent with HHV-6A being a cofactor in the pathogenesis of MS, in some people. If infection with both EBV and HHV-6A are synergistic, what might be the mechanisms? HHV-6A (but not HHV-6B) can coinfect B cells latently infected with EBV, and transactivate EBV. HHV-6A lytic infection of oligodendrocytes (myelin-producing cells) could compromise remyelination when an autoimmune process has produced demyelination. HHV-6A proteins and lipids may incite autoimmunity; indeed, one HHV-6A peptide reportedly has the potential for generating autoantibodies against myelin basic protein.
Claims that many different specific viruses are causes of MS have failed replication over the past century. Currently, evidence linking EBV to MS is strong, evidence for HHV-6A is growing stronger, and some evidence suggests that endogenous retroviruses (or their gene products) may also play a role in some cases.