Patients with viral loads suggestive of iciHHV-6 had the greatest risk of developing demyelinating disease.
Considerable evidence indicates that infection with Epstein-Barr virus, particularly in the first several years after primary infection, contributes to the pathogenesis of multiple sclerosis. Perhaps the most impressive are a 2022 longitudinal study in over 10 million military recruits finding a greatly increased risk of multiple sclerosis, a common example of demyelinating disease (Bjornevic 2022), and a study providing convincing evidence of molecular mimicry as a mechanism for pathogenesis (Lanz 2022).
However, there also is considerable evidence that HHV-6 may contribute, in some people, to the pathogenesis of the multiple sclerosis, alone or in combination with EBV (Soldan 2001, Leibovitch 2018, Engdahl 2019, Bistrom 2021, Wu 2022, Komaroff 2020).
Australian investigators studied 204 people with first episodes of central nervous system demyelination, and compared them to 215 healthy control subjects matched for age, gender, and geographic region of residence. Whole blood viral load of HHV-6 and VZV and various antibody levels for HHV-6, VZV and CMV were measured.
After a multivariate analysis that adjusted for education, 25(OH)-vitamin D levels and smoking history, only two factors correlated with the development of demyelinating disease: presence of HHV-6 DNA in whole blood (adjusted odds ratio=2.2, CI 1.08-4.46), and increased levels of EBV-EBNA-IgG in serum. Patients with both of these factors had the highest likelihood of developing demyelinating disease (see Table).
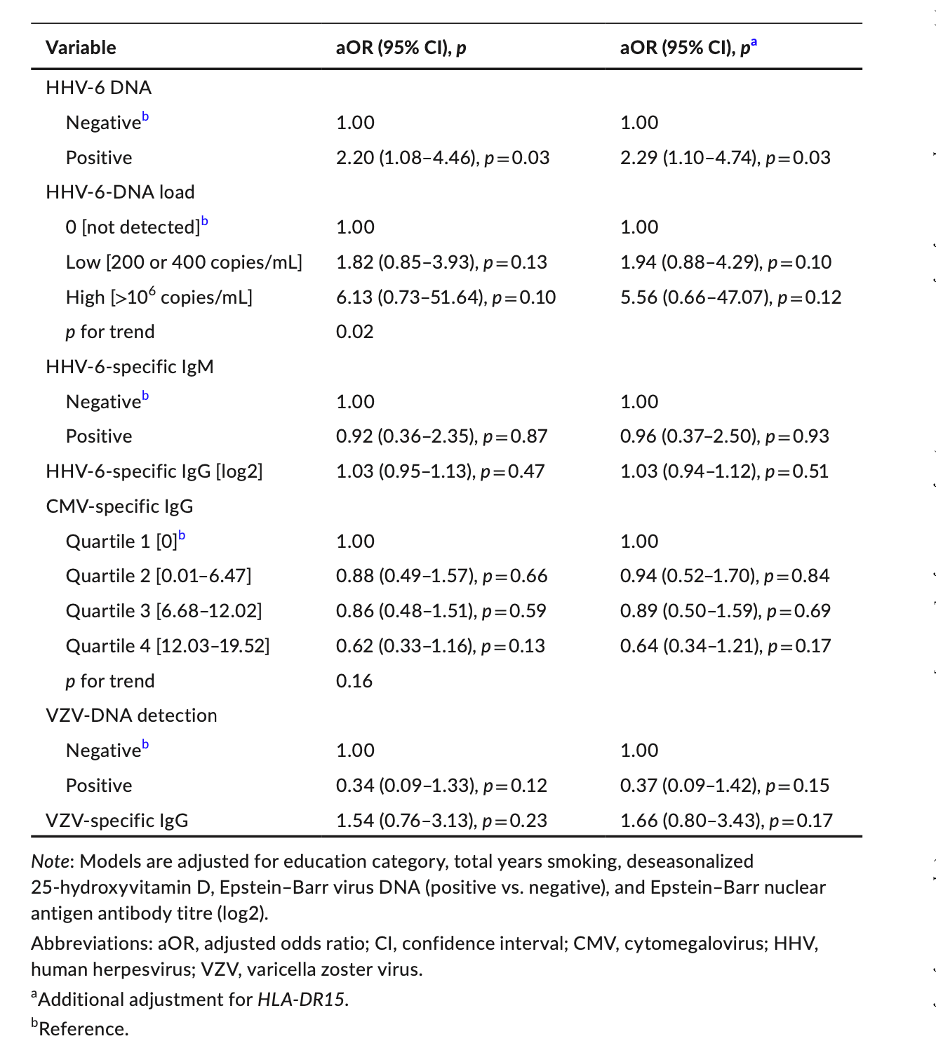
Table 1. Results of multivariable conditional logistic models of the association between viral markers and risk of first clinical episodes of demyelination.
Of interest, six cases out of 204 (2.9%) had HHV-6 extremely high viral loads (> 5.5 log 10 copies/ml) presumably representing inherited chromosomally integrated HHV-6 (iciHHV-6) (Pellett 2012). These patients also had the highest likelihood of developing demyelinating disease (a six-fold increase in odds ratio). Moreover, multivariable conditional logistic models that adjusted for education, 25(OH)D concentration, smoking, EBNA IgG (log2), and EBV-DNA load (positive vs. negative) found that only the HHV-6-DNA load was significant in discriminating cases from controls.
Only a fraction of the HHV-6 positive samples were genotyped, and most were determined to be HHV-6B. HHV-6A (but not HHV-6B) has been found in the serum of MS patients undergoing relapse (Alvarez-Lafuente 2006).
Despite the limitations of this study, it is consistent with others that have found evidence that HHV-6A/B may contribute to the pathogenesis of demyelinating diseases, particularly multiple sclerosis.
Read the full article: Lucas 2023