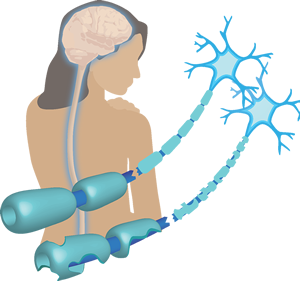
A group led by Margot Mayer-Proschel, Ph.D and David Mock, MD has broken new ground in the understanding of HHV-6’s role in demyelinating diseases like Multiple Sclerosis (MS). Their experiments revealed that the HHV-6A latency gene, U94, inhibits migration of cells critical for myelin repair, known as oligodendrocyte progenitor cells (OPCs). A strong migration and differentiation response is needed to repair myelin that has been damaged during demyelinating insults. It is also thought that an inefficient myelin repair in MS is associated with progression of the illness from a relapsing-remitting state to a chronic disease often accompanied by secondary neuronal damage and cognitive impairment . The ability of HHV-6A to impede the normal repair process suggests that it could be involved in the progression of MS, and raises questions about the virus’s role in other chronic demyelinating diseases as well.

Margot Mayer-Proschel, PhD, University of Rochester Medical Center
In the study, Drs. Mayer-Proschel and Mock’s team first analyzed human oligodendrocyte progenitor cells (hOPCs) expressing the HHV-6A U94 gene in vitro, finding that these cells displayed impaired migration when compared to controls. This effect was then confirmed in vivo using mice with extensive myelin loss. Twenty-one days after injection of hOPCs into the hippocampus and the corpus callosum, the brains were harvested, and impaired migration of the U94A+ cells was demonstrated in both brain regions. Importantly, the effect was not attributed to decreased cell survival or proliferation. Differentiation of the hOPCs into GFAP+ astrocytes or GalC+ oligodendrocytes in vitro was also not significantly affected by U94 expression.
Notably, a role of U94 in host cell function does not appear to be specific to hOPCs. In 2009, U94 was shown to inhibit formation of in vitro capillary-like structures, migration of endothelial cells, and angiogenesis (Caruso 2009). Recently, another team suggested a role of U94 in reduction of tumor cell growth, invasion, and metastasis (Caccuri 2017). Our growing understanding of the functions of HHV-6 U94 may provide insight into the mechanisms behind HHV-6-associated diseases, and may harbor the potential for development of new therapies.

Co-author and “spark plug” for the University of Rochester study David Mock, MD, who has been studying HHV-6 and demyelination since 1999, at the 10th International Conference on HHV-6 & 7.
In light of the results presented by the Rochester team, the authors caution against use of primary hOPCs for therapeutic transplantation approaches without first testing for the presence of latent HHV-6 infection. While it is difficult to target a latent HHV-6 infection, targeting specific viral proteins and inhibiting their function might also offer a new avenue for antiviral therapy to control the adverse effects of latent infections.
Find the full paper here: Campbell 2017.
Read the University of Rochester press release here.