Study results are consistent with a pathogenetic role for viruses in relapsing-remitting MS.
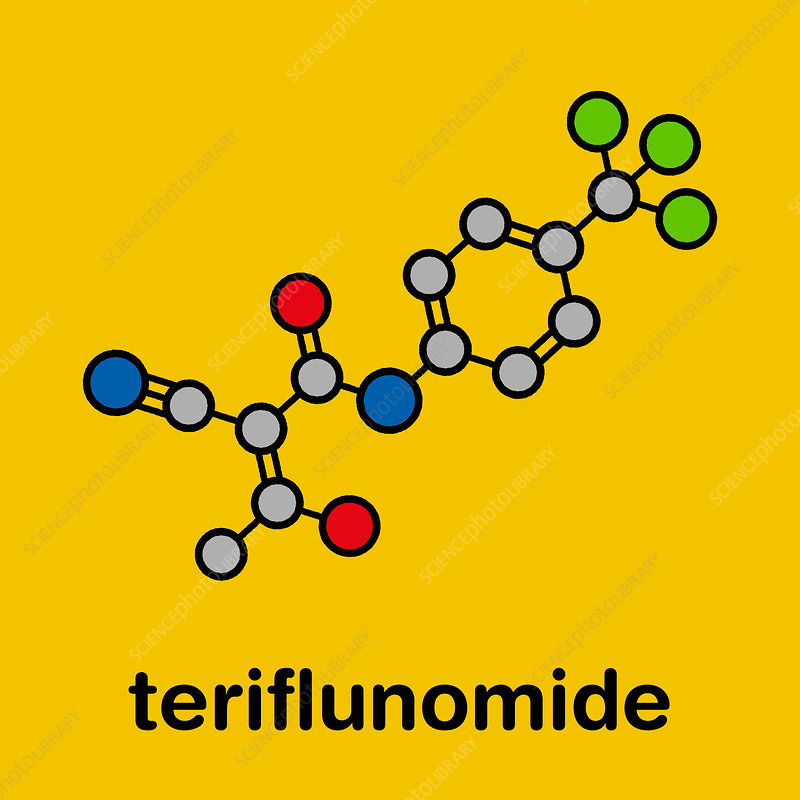
Both EBV and HHV-6A have been incriminated as possible triggering agents of relapsing-remitting multiple sclerosis (RRMS). RRMS, in turn, responds to orally-administered teriflunomide, an immunomodulator drug with broad-spectrum antiviral properties. Previous animal and in vitro studies have suggested that this drug may has antiviral properties against multiple viruses including SARS- CoV-2, RSV, EBV, CMV and BK virus in vitro and promotes apoptosis in EBV transformed cells (Lang 2023, Bilger 2017, Dunn 2010).
A multi-center prospective study was conducted in Spanish hospitals to evaluate the response to teriflunomide therapy. Specifically, antibody levels against EBV and HHV-6, evidence of neuronal injury (through determining levels of serum neurofilament light chain protein, or Nf-L) and clinical remission (no evidence of relapses, disability progression, or new lesions on MRI scans) were measured. Serum samples were obtained before and for at least 6 months after treatment was started. Ultimately, 90 people completed the study.
The main results of the study were:
- Antiviral antibody levels declined substantially after 6 months of treatment: EBNA-1 IgG (down 74%), VCA IgG (down 69%), HHV-6A/B IgG (down 60%), and HHV-6A/B IgM (down 73%);
- The drop in these antiviral antibody levels was greater than was found by previous studies using other immunomodulator drugs used to treat RRMS;
- EBV-VCA IgG titers at baseline correlated with Nf-L levels measured at the same time (r = 0.221; p = 0.028) and 6 months later (r = 0.240; p = 0.017), linking EBV more strongly to evidence of neuronal injury;
- Nevertheless, a positive correlation that nearly achieved statistical significance also was seen between neuronal injury and elevated levels of HHV-6A/B IgM at baseline and after 6 months of treatment, and the study might have been underpowered to recognize the correlation as significant;
- After 2 years of treatment with teriflunomide A, 45% of patients had no evidence of clinical progression; however, 14.4% (13/90) had therapeutic failure;
- The patients who were most likely to respond to teriflunomide therapy were older, had longer-lasting disease, higher EBNA-1 titers, and a lower number of gadolinium-enhanced lesions on MRI scans.
This study, like others, suggests that EBV, and possibly HHV-6A, may contribute to the pathogenesis of RRMS. Antibody levels to both EBV and HHV-6 were correlated with evidence of neuronal injury, although the evidence was stronger for EBV.
RRMS is an immunologically-mediated disease but this immunomodulator’s broad spectrum antiviral properties may contribute to the clinical benefit observed in this and other studies. Similarly, beta interferon, an immunomodulator used for decades against multiple sclerosis, inhibits both HHV-6 and EBV in vitro and in vivo (Garcia-Montojo 2007, Sedaghat 2022).
Unfortunately, teriflunomide therapy does not stop disease progression in all patients with RRMS.
Read the full article: Dominguez-Mozo 2023