Berzero et al. of the University of Pavia, Italy, evaluated all 926 patients at their institution who were tested for HHV-6 DNA in the cerebrospinal fluid (CSF) and/or blood over a decade: 45 tested positive. Of the 17 immunocompetent patients, 4 were diagnosed with HHV-6 encephalitis, all of whom were infants younger than 3 years old. Of the 28 immunocompromised hosts, 7 were diagnosed with HHV-6 encephalitis: most were adults (two were teenagers) and in all cases the encephalitis was caused by reactivation of the virus.
The authors compared the ratio of viral load in the CSF to the viral load in the blood: they found that this “HHV-6 CSF/blood replication ratio” was >1 in 6/7 of the immunocompromised patients, whereas it was <1 in all 4/4 immunocompetent patients. They conclude that the detection of a CSF/blood replication ratio >1 represents a specific feature of immunocompromised patients with encephalitis.
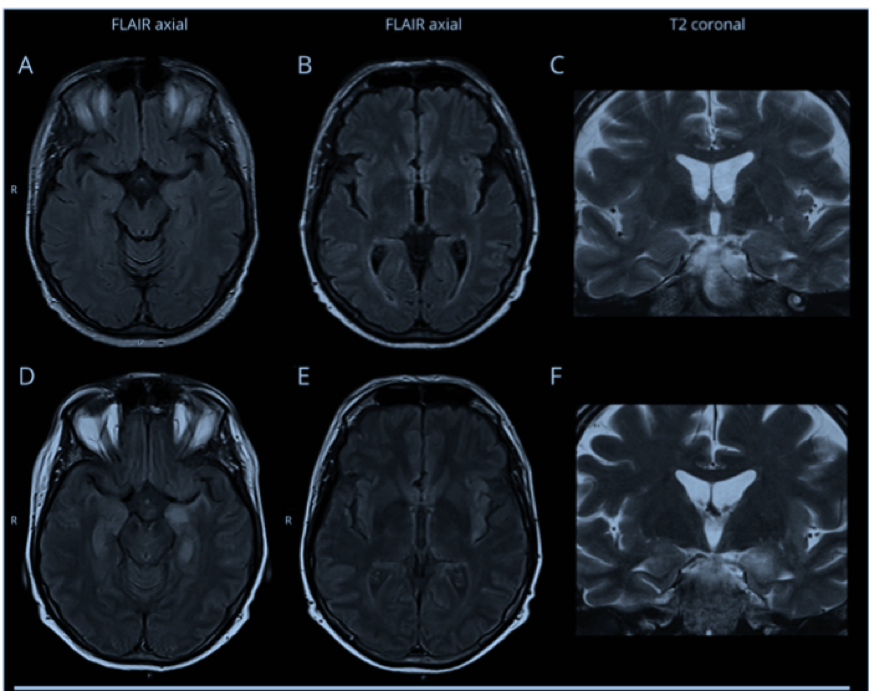
MRI changes in an HSCT patients with encephalitis are often delayed. Panels A-C represent MRI 3 days after symptom onset with no abnormal findings on axial FLAIR and coronal T2-weighted images with motion artifacts. 16 days after symptom onset, a marked hyperintensity was evident at the level of the left temporo-mesial region with swelling of the amygdala and ipsilateral insular cortex, panels D-F.
For one HHV-6 patient, no abnormal findings were detected on MRI 3 days after initial symptom onset (Fig 1A-C). It was only an MRI 16 days later that revealed abnormalities (Figure 1D-F). Thus, a negative brain MRI performed shortly after symptom onset does not rule out HHV-6 encephalitis.
Finally, the authors detected inherited chromosomally-integrated HHV-6 (iciHHV-6) in 7/926 (0.8%) of all patients tested, a proportion similar to that in the general population (Pellett 2012).
Read the full article: Berzero 2021