Chinese investigators found a high prevalence of HHV-6 and Epstein Barr virus in the brain tissues of children with Rasmussen’s encephalitis but in none of the controls. There was a significant association between viral presence and brain atrophy, raising a strong suspicion for the involvement of both viruses.
Rasmussen’s encephalitis is a condition affecting children that is marked by seizures and cognitive deterioration. Previously, HSV, EBV, and CMV antigens and DNA have been detected in RE tissues but have not accounted for all patients.
The Chinese study employed immunohistochemical staining to detect EBV and HHV-6 antigens in brain tissue from 30 patients (mean age at surgery of 6.8 years) with RE who had undergone craniotomy, as well as 16 control patients (mean age at surgery of 8.2 years) who had undergone surgical treatment for cerebral trauma. Antibodies against EBV latent membrane protein 1 (LMP1) and HHV-6B late antigen p101K were used to determine the prevalence of either virus in tissue sections, and expression levels of these proteins were analyzed by determining the percentage of antigen-positive cells and assessing staining intensity by color. In total, EBV LMP1 was present in 17/30 (56.7%) of RE patients, and HHV-6B antigen was present in 15/30 (50%). Of the positive cases, 7 exhibited moderately-strongly positive staining for HHV-6 antigen, while 8 cases showed weakly positive staining. EBV was moderately-strongly positive in 4 cases and weakly positive in 13. Only 2 of 15 HHV-6+ cases did not exhibit brain atrophy while 10 of 15 HHV-6- samples showed no atrophy. Double immunofluorescence staining revealed that both types of antigens were localized in the cytoplasm and/or nuclei of neuron-like cells in lesion areas of RE brains. Zero controls exhibited any staining toward either virus.
MRI results revealed that the patients who were positive for HHV-6B and EBV antigens had more severe brain atrophy (p=0.008 and p=0.002, respectively) than those who were negative. Additionally, the 6 patients with HHV-6/EBV coinfections all had a high grade of brain atrophy, suggesting that coinfection may result in more severe neuronal damage.
One patient in particular was detailed in the report: a 4-year-old boy with a typical RE course who displayed HHV-6/EBV coinfection. The boy was first diagnosed with “viral encephalitis”, but after initial medication-induced improvement in symptoms subsequently worsened, he was given a diagnosis of RE a year later. HHV-6 and EBV were detected in both neurons and, as has also been seen in the brains of patients with mesial temporal lobe epilepsy (Fotheringham 2007), in astrocytes. Infiltration of a large number of cytotoxic CD8+ T cells was found near neurons, and pyknosis, neuronal loss, perivascular lymphocyte cuffing, and glial cell proliferation were also seen in the temporal lobe cortex. The proximity of the CD8+ T cells to neurons led the authors to postulate that the dual viral infections triggered an influx of the lymphocytes, which targeted infected cells and consequently damaged neurons, thereby leading to brain atrophy. Furthermore, the authors suggest that absence of viral detection in some cases of RE may be a result of an infection that has already been cleared by the immune cells that flood the area.
In the case of the 4-year-old boy, the time between initial diagnosis of viral encephalitis and the eventual diagnosis of RE suggests that earlier treatment for HHV-6 and EBV, when the patient was first admitted for repeated fever and convulsions, may have lessened the CD8+ infiltration and significant brain atrophy. Especially as the immune response, rather than primarily direct virus-induced cell death, may ultimately result in the brain atrophy present in RE, early antiviral treatment could be essential to treating the condition; When significant brain atrophy is already present, antiviral treatment may be relatively ineffective. In cases of “viral encephalitis” in children, testing/monitoring for and treatment of HHV-6 and other herpesviruses might result in fewer cases of RE down the road. For such a serious disease, for which treatment for controlling seizures and cognitive deterioration is often hemispherectomy, new ways to identify cases early and develop new methods of treatment are essential.
One small study also detected HHV-6 DNA by nested PCR in 2/3 RE patients; one of these HHV-6+ patients had an HSV-1 coinfection, and the other was triple-infected with HSV-1, CMV, and HHV-6 (Eeg-Olofsson 2004). An earlier report found weak positivity for HHV-6 by qualitative PCR in 1/7 RE patients (Vinters 1993). In light of the present study, it appears that HHV-6B may cause or contribute to a subset of cases.
For more information on HHV-6 in encephalitis, visit our web page on the subject: HHV-6 & Encephalitis.
Find the full paper here: Liu 2018.
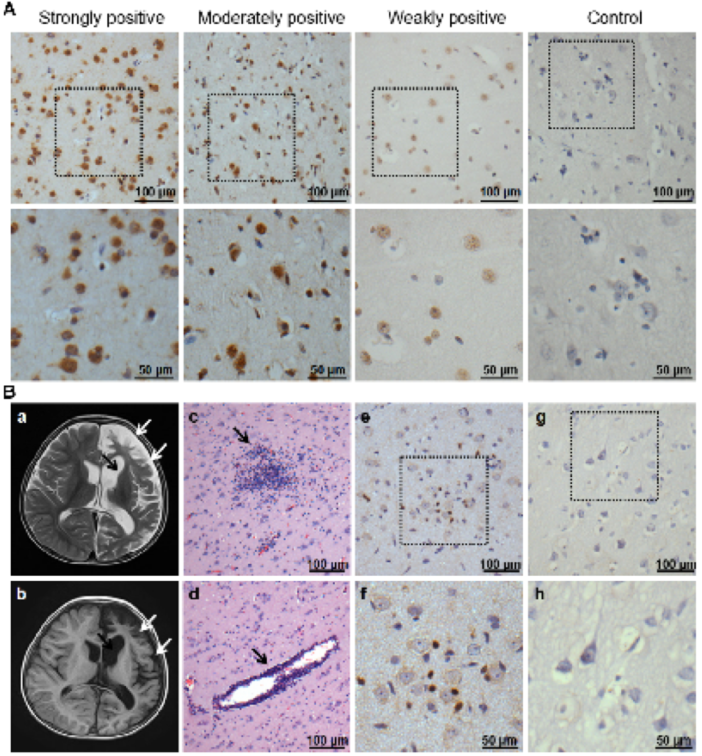
HHV-6 expression in brain tissues of patients with RE and controls. A) Representative images B) Atrophy of the left hemisphere cortex widening of the caudate nucleus. HE shows microglial nodule formation, lymphocyte infiltration and perivascular cuff. Activation of CD8+ T cells were detected in RE but not in brain tissue from a trauma patient.

