Latvian researchers studied autopsy material from the olfactory bulb and tract region of the brain in controls as well as patients with HHV-6 associated encephalopathy. Distinctive structural alterations of oligodendrocytes, cells responsible for the production and maintenance of myelin, were found. In addition, the group found pathological changes in the myelin sheath of axons in the HHV-6 DNA+ samples by electron microscopy.
The team, led by Modra Murovska from the Riga Stradins University, determined that HHV-6 viral loads in olfactory bulb tissue samples from autopsies of 20 patients with unspecified encephalopathy were significantly higher than in 17 age-matched controls or 16 younger controls. The prevalence of HHV-6 in diseased tissues of the olfactory tract/bulb was 60%- higher than in the tissues of both age-matched controls (29%) and younger controls (19%). Additionally, significantly more HHV-6+ oligodendrocytes, astrocytes, microglia, and endothelial cells were found in the white matter of encephalopathy patients than in controls.
Strong evidence of a role for HHV-6 in unspecified encephalopathy came from the ultrastructural changes found via electron microscopy in the olfactory pathways of these patients, but not in any control tissues. Overall, the characteristic finding among these samples was widespread myelin changes. Consequently, the data produced in this study provides important insight into the role of HHV-6 in other demyelinating conditions, especially MS (Alenda 2014).
Immunohistochemical analysis revealed that compared to both control groups, the encephalopathy group had a higher number of HHV-6+ astrocytes (p=0.005) in the gray matter, and a higher number of both HHV-6+ astrocytes and oligodendrocytes (p<0.001) in the white matter. Moreover, HHV-6+ encephalopathy cases were positively correlated with the more cytotoxic CD8+ cells as opposed to helper CD4+ cells.
There were also higher levels of activated microglial cells in the white matter than in the gray matter, leading the investigators to conclude that the white matter is more actively involved in the pathological processes of unspecified encephalopathy.
Intriguingly, the investigators also found that HHV-6 positivity was associated with lower levels of S100 positive cells. S100 proteins are markers for inflammatory disease and cancer. The authors speculate that reduced S100 expression may result from depletion of intracellular resources due to long standing infection.
Structural alterations were also seen in endothelial cells, pericytes (the contractile cells that wrap around the endothelial cells of capillaries), and venules, as well as in the basement membrane in the HHV-6+ tissues of those with encephalopathy.
The group proposes that HHV-6 may contribute to unspecified encephalopathy in middle-aged and older patients through ongoing neuroinflammation and demyelination resulting from reactivation of latent infection.
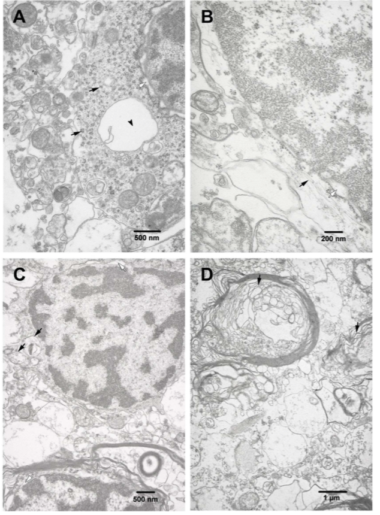
Ultrastructural changes in the olfactory pathways of HHV-6+ patients. Source: PLOS ONE
A latent infection of HHV-6 has often been thought to be innocuous. The results from this study, however, suggest to the authors that over time, latent HHV-6 infections may produce significant damage. This data is supported by a 2014 animal model that showed that HHV-6A is able to induce neuroinflammation in the absence of replication (Reynaud 2014) in transgenic mice.
HHV-6A and –B have been associated with several neurological disorders, including MS, encephalitis, febrile seizures, and temporal lobe epilepsy. Additionally, HHV-6 can cause acute encephalopathy, particularly during primary HHV-6B infection and post-transplantation, but also in those with a genetic predisposition.
Find the full paper here: Skuja 2017

