In the past two decades, there has been increasing evidence that chronic infection of the brain by neurotropic viruses, particularly herpesviruses, may be one trigger for dementia. Herpes simplex virus type 1, in particular, has been linked to dementia (Itzhaki 2020), as have other herpesviruses, including HHV 6, as summarized in a relatively recent review (Komaroff 2020). A recent study involving a large number of subjects examined the possible connection between chronic viral infection and the development of subsequent dementia.
Of the 500,000 individuals with medical history data and biosamples in the UK Biobank, over 9,000 were tested for antibodies to 15 viruses: HSV-1; HSV-2; Varicella Zoster virus; Epstein-Barr virus; Human Cytomegalovirus; HHV-6; HHV-7; Kaposi sarcoma-sssociated herpesvirus; Hepatitis B virus; Human T-Lymphotropic Virus 1; Human Polyomavirus BKV; Human Polyomavirus JCV; Merkel Cell Polyomavirus; Human Papillomavirus type-16; Human Papillomavirus type-18. Hepatitis C virus and HIV-1 had such low seroprevalence that they were not studied.
The investigators examined the possible correlation between serological evidence of infection with each of these viruses, individually, and the subsequent development of dementia about a decade later. As shown in the table below, only for HSV-1 was the correlation with subsequent dementia statistically significant: (OR 2.14, 95% C.I. 1.20–3.81). Correlations that almost reached statistical significance were also seen for VZV and HHV 6.
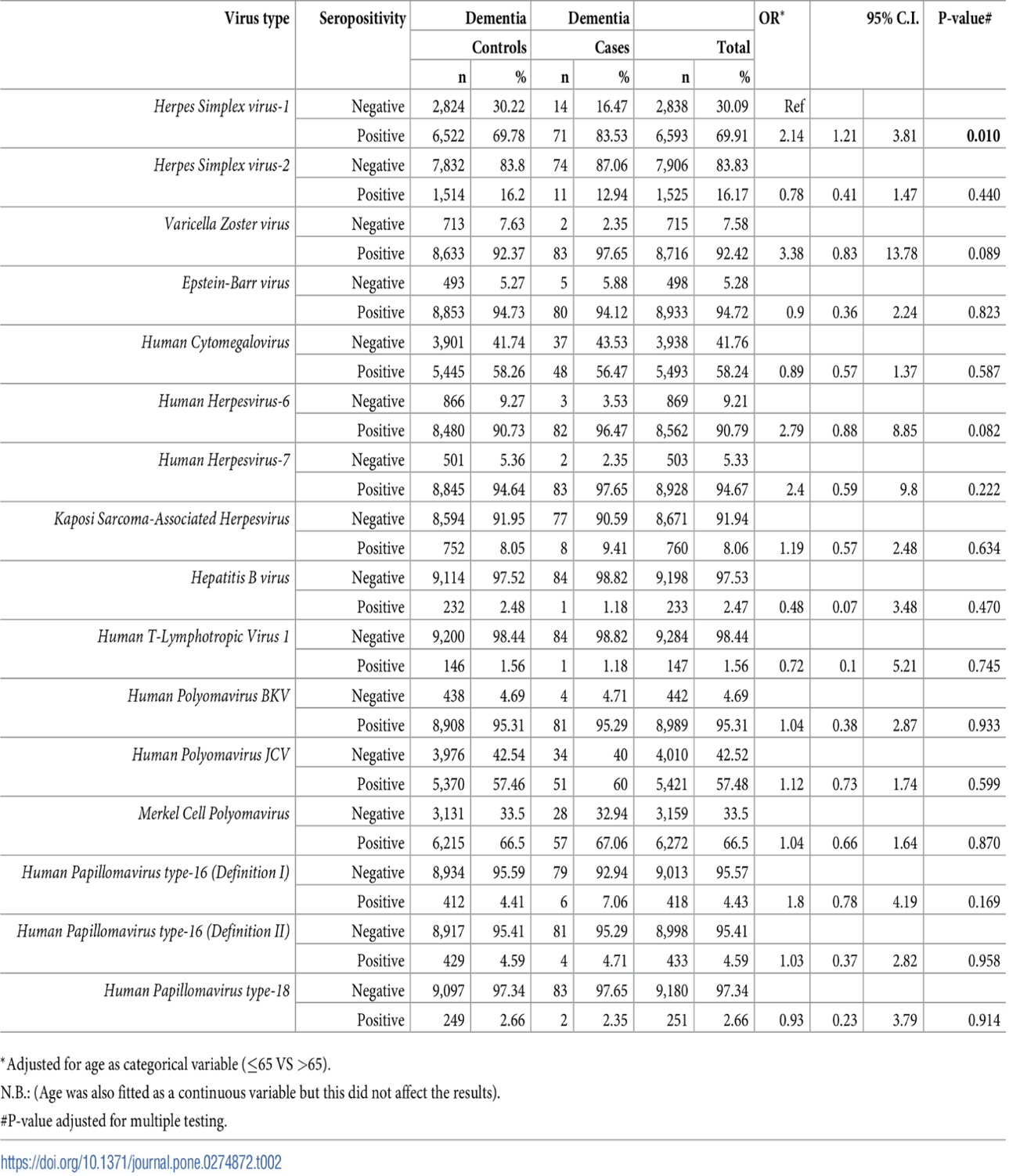
Table - Associations between seropositivity for IgG antibody measures and dementia risk.
However, the investigators decided a priori to also examine the risk of subsequent dementia in individuals who were seropositive for all four of the following herpesviruses: HSV-1, VZV, HHV-6 and HHV-7. Individuals seropositive for all four viruses had a highly statistically significant correlation with the subsequent development of dementia: (OR =2.37 95% CI 1.43-3.92).
The authors do not state whether the over 9,000 individuals on whom serological studies for viruses were conducted were representative of the larger population of over 500,000 people in the UK Biobank, nor whether the people in the UK Biobank are representative of the population of the UK. The authors also do not state what the definition of “seropositivity” was for each virus: antibodies against which specific viral antigens; was there a threshold level of detectable antibody above which a study subject was deemed “seropositive”; was any attempt made to correlate the level of seropositivity to the risk of subsequent dementia?
Despite these concerns, the study provides some support for the theory that chronic infection of the brain, presumably by provoking a chronic low-level inflammatory response, may be one trigger for dementia, including Alzheimer’s disease.
Read the full article Mekli 2022

