HHV-6 reactivation is a relatively common occurrence after allogeneic hematopoietic stem cell transplant (alloHSCT). Certain factors such as cord blood transplantation are risk factors for HHV-6 reactivation and more serious events like HHV-6 encephalitis (Yamane 2007). However, HHV-6 reactivation is relatively undocumented following unmanipulated haploidentical HSCT (haploHSCT)—transplants from donors (often family members) who are half HLA-matched, used when fully-matched donors are unavailable.
Han et al. used novel granulocyte-colony stimulating factor (G-CSF)-mobilized bone marrow and peripheral blood cells as the source of stem cells in haploHSCT, and measured HHV-6 reactivation repeatedly for 100 days following transplantation.
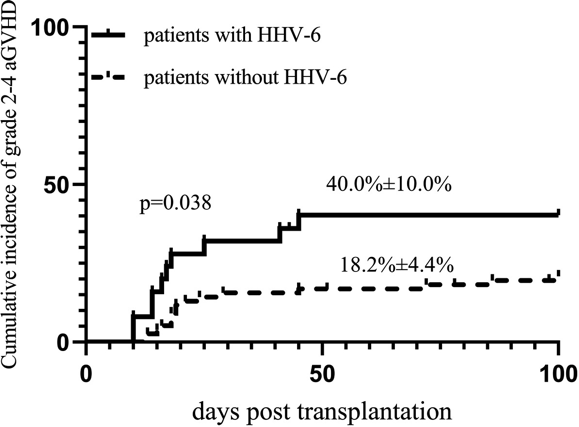
Figure 1 - Cumulative incidence of grade 2-4 aGVHD in patients with and without HHV-6 viremia (Han 2021)
At day-100 post-HSCT, the cumulative incidence of HHV-6 reactivation was 25.5%. Of the patients with reactivation of HHV-6, 40% of patients exhibited acute graft versus host disease (aGVHD). Of the patients who did not reactivate HHV-6, only 18.2% developed aGVHD (P=0.038) (Figure 1). By multivariate analysis, prior HHV-6 viremia was an independent risk factor for the development of grade 2-4 aGVHD.
Thus, this study finds that in haploidentical hematopoietic stem-cell transplant using granulocyte-colony stimulating factor (G-CSF)-mobilized bone marrow and peripheral blood cells, the occurrence of HHV-6 reactivation is associated with a substantially increased risk of aGVHD as it is in other forms of allogeneic hematopoietic stem-cell transplantation. The important question not addressed by this study is whether antiviral treatment of HHV-6 reactivation would reduce the risk of aGVHD.
The study did not find statistically significant differences between those patients with HHV-6 reactivation and those without in overall survival, disease-free survival or non-relapse mortality. However, the number of subjects who were studied was small and the statistical power of this study was poor, thus precluding any conclusions about survival.
Read the full article: Han 2021

