As with previous studies, HHV-6 reactivation delayed platelet engraftment and increased the risk of aGVHD.
The frequency and clinical importance of HHV-6B reactivation can be different, following alternative kinds of hematopoietic cell transplantation (HCT). A study from France is one of the largest to study HHV-6 reactivation in adults following unmanipulated T-cell replete haplo-identical (HAPLO) HCT with post-transplant cyclophosphamide (PT-Cy), plus or minus pre-transplant low-dose rabbit anti-thymocyte globulin (ATG).
The study involved 100 consecutive adult patients receiving HAPLO HCT with PT-Cy, some of whom also received pre-transplant ATG as part of their clinical care. The patients had venipunctures every week for the first 100 days post-HCT, regardless of whether they were symptomatic, in order to assess reactivation of HHV-6B (DNA loads) and other viruses using quantitative PCR. Regular venipunctures continued thereafter if indicated by the patients’ clinical status.
The main results of the study are as follows:
- Patients experiencing HHV6 reactivation demonstrated delayed platelet recovery (HR 1.81, 95% CI 1.07-3.05, p= 0.026) and a higher risk of acute grade II-IV GvHD (39% versus 9%, p < 0.001); however, they had similar overall survival and non-relapse mortality to the other patients. A low absolute lymphocyte count (ALC) was a risk factor for this complication, as shown in Figure 1.
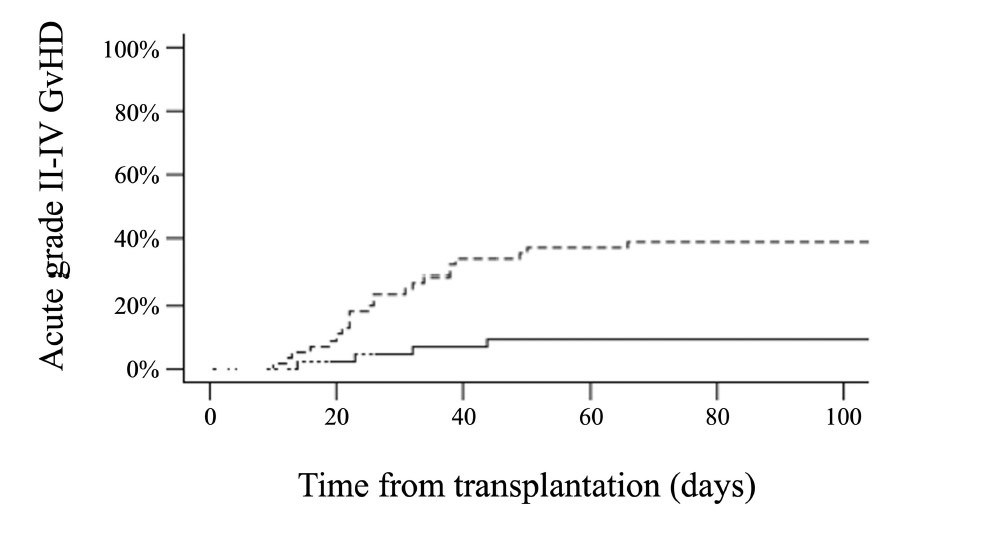
Figure 1. Cumulative incidence of acute grade II-IV GvHD according to HHV6 reactivation within 100 days after haploidentical hematopoietic cell transplantation with post-transplant cyclophosphamide (dashed line: HHV6 reactivation, continuous line: no HHV6 reactivation). The cumulative incidence of acute grade II-IV GvHD at day +100 was 39% versus 9% (p < 0.001).
- A low absolute lymphocyte count (< 290/µL on day +30) also was the main risk factor for
HHV6 reactivation (68% versus 40%, p = 0.003).
- The 100-day cumulative incidence of HHV6 reactivation was 54% — a rate similar to that following HCT with matched related or unrelated donors, and lower than the rate following umbilical cord transplantation.
- The rate of HHV-6 reactivation reported may have been lower than it otherwise would have been since antiviral therapy against CMV was used in a large fraction of the patients.
- Clinically significant HHV6 infections were rare (7%), were associated with higher HHV6 DNA loads, and had favorable outcomes after antiviral therapy.
- Although there were theoretical reasons for worrying that it might, adding ATG to PT-Cy did not increase the incidence of HHV6 reactivation (52% with ATG versus 79% without ATG, p = 0.12).
A key strength of this systematic study of HHV-6 reactivation in adults receiving HAPLO HCT with PT-Cy is its weekly monitoring of HHV-6 viral loads, regardless of the patients’ clinical status. The findings of greatest interest to clinicians may be the demonstration that combining ATG and PT-Cy does not increase the risk of HHV6 reactivation or infection. In addition, the study suggests that patients with a low ALC on day +30 face a higher risk of HHV6 reactivation and may require more intense monitoring.
Read the full text: Paviglianiti 2024