Odds of mortality were 2.6-3X higher in patients with detectable viral DNA; odds were even higher with multiple herpesviruses.
Sepsis is the leading cause of death in children worldwide. Small studies in the past have suggested that the prognosis is worse when children with sepsis have evidence of reactivated DNA viruses, particularly herpesviruses (Davila 2018). A much larger, multi-center study of 401 children hospitalized in an intensive care unit (ICU) found that viremia was associated with significantly increased odds of mortality and that the odds increased further when multiple herpesvirus infections were detected. HHV-6 was the most common virus found in these patients (other than TTV which was ubiquitous and not associated with increased mortality).
24% (93/431) of the patients had plasma samples positive for HHV-6 DNA compared to 13% and 14% for CMV and EBV. While 11% of the 401 patients died, the mortality rate for those with two or more viruses was 19.5%. The median age was 6 (IQR, 1-12) years; 222 (55.4%) were male. One hundred fifty-four patients (38.4%) were previously healthy, 108 (26.9%) were immunocompromised, and 225 (56.1%) had documented infection(s) at enrollment.
The earliest available plasma sample day from each patient’s ICU stay was tested for both DNAemia of the 8 viruses and IgG antibodies to CMV, EBV (viral capsid antigen), HSV-1, and HHV-6. DNA was tested using quantitative real-time polymerase chain reaction (qPCR) assays (R-gene; bioMérieux) for the following viruses: CMV, EBV, HSV-1, HHV-6, parvovirus B19, BK polyomavirus (BKPyV), human adenovirus (HAdV) and torque teno virus (TTV). Serologic testing was performed using multiplex flow immunoassays (BioPlex 2200 system; BioRad) except for HHV-6, which was tested using an indirect fluorescence assay (SCIMEDX Corporation).
Forty-four of the patients (11.0%) died in the ICU. Viral DNAemia with at least 1 virus (excluding TTV) was detected in 191 patients (47.6%) overall—58.3% of whom were immunocompromised at the onset of sepsis.
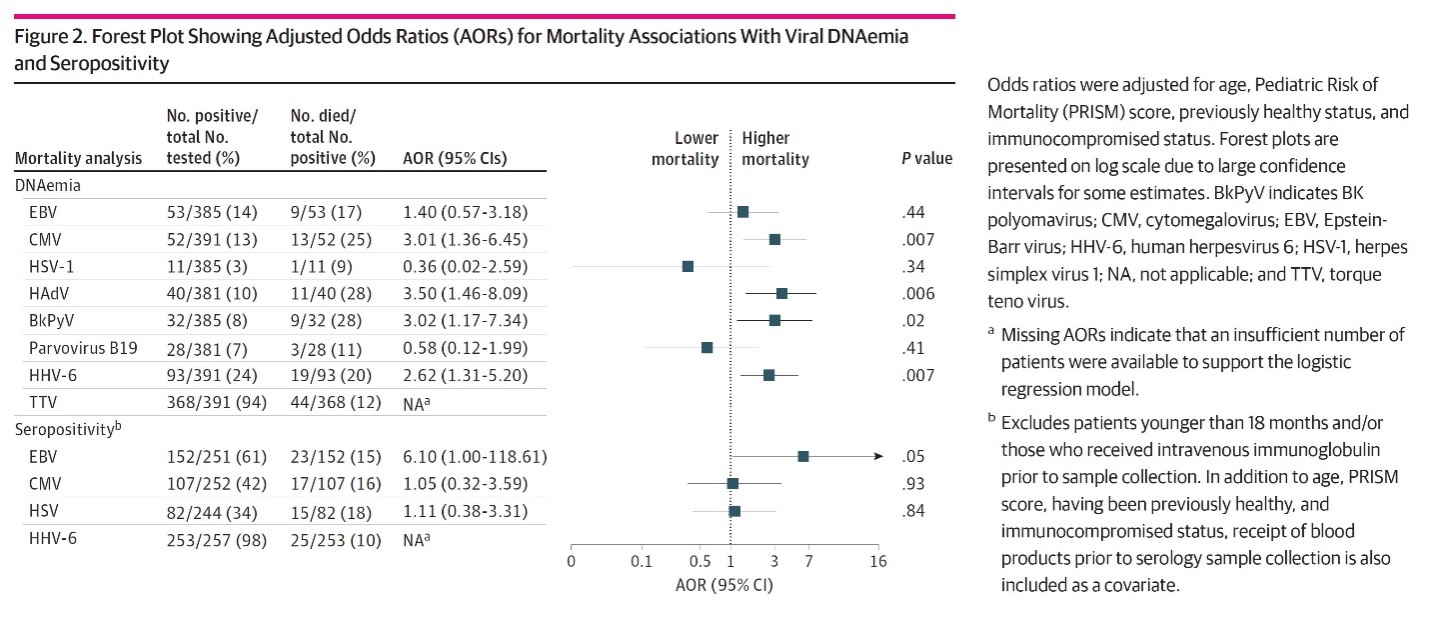
Multivariable statistical analysis then was used to assess whether evidence of latent or reactivated DNA viral infection was associated with the risk of mortality. After adjustment for age, Pediatric Risk of Mortality score, previously healthy status, and immunocompromised status at sepsis onset, DNAemia with CMV, HAdV, BKPyV, and HHV-6 were significantly associated with increased mortality, as shown in the figure, below. Detecting DNAemia involving two or more viruses also was associated with increased mortality. (Since virtually all subjects had evidence of detectable TTV DNA, the meaning of this result was difficult to ascertain.)
This study tacitly assumed that detection of viral DNAemia reflected reactivation from latency and production of new virus. However, it is possible that sepsis could have led to release of nonviable viral DNA from latently infected cells.
Finally, EBV seropositivity was marginally associated with an increased risk of mortality; seropositivity for the other herpesviruses were not associated with increased risk.
In summary, this study demonstrates that detecting DNAemia from several DNA viruses—particularly CMV, HAdV, BkPyV, and HHV-6—is associated with a clearly increased risk of death in pediatric patients requiring intensive care for sepsis. The study begs the question, however, of whether the association is causal, or whether the DNAemia is simply an epiphenomenon—a biomarker of compromised immunity.
An efficient way to distinguish whether the CMV, HAdV, BkPyV, and HHV-6 DNAemia cause increased mortality would be controlled studies of antivirals in those with DNAemia. Two small studies of ganciclovir treatment for adult ICU patients with CMV infection have been conducted; while the viral load was reduced and there were fewer days on the respirator, there was no reduction in IL-6 levels or mortality (Limaye 2017, Papazian 2021) . Ganciclovir is also immunosuppressive, and use of newer, less toxic antivirals might have had improved the outcome. The results of this study in children suggest the value of a controlled trial of antiviral therapy in cases of sepsis with DNAemia.
Read the full article: Cabler et al. 2024

