Lee et al., of the infectious disease service at Weill Cornell, prospectively analyzed a cohort of adult ex vivo T-cell depleted (TCD) hematopoietic cell transplant (HCT) recipients from 2012-2016. Quantitative PCR was used to monitor the patients every 1-2 weeks from day 14 to day 100 post-transplant.
Of the 312 patients enrolled, 83 (27%) had persistent HHV-6 DNAemia (p-HHV-6) by D+100, indicated by ≥ 2 consecutive values of ≥ 500 copies/mL. Patients with p-HHV-6 had lower platelet count (PLT) (p=0.014) and lower absolute lymphocyte count (ALC) (p<0.0001), CD4+ (P = 0.0002) and CD8+ (p=.024) lymphocyte counts at D+100. Multivariable analysis estimated that detecting p-HHV-6 was independently associated (after adjusting for cell counts and other potential confounders) with reduced overall survival (58.8% vs 79.4%, respectively; P=0.0001).
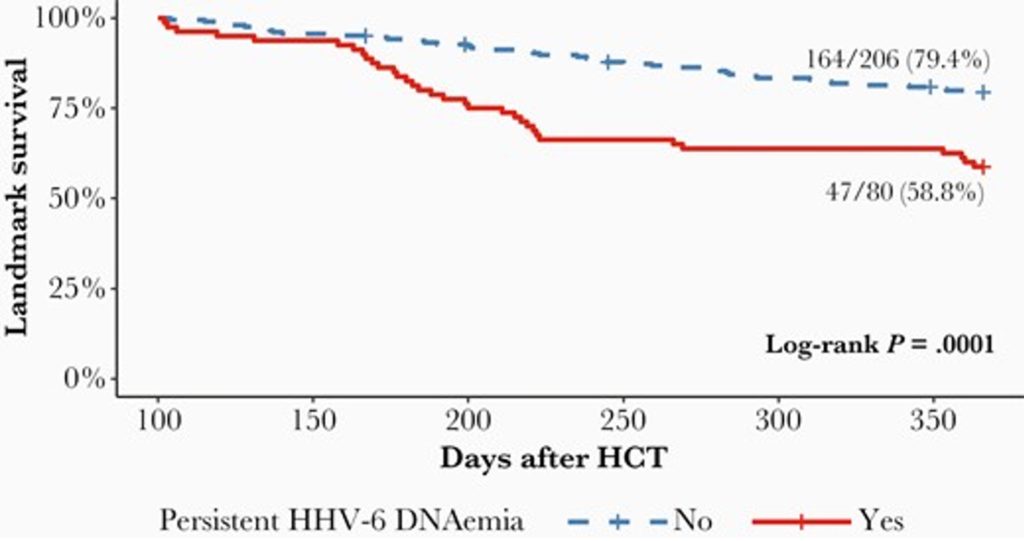
Survival analysis from D+100 through 1-year post HT. Only patients alive at D+100 were included. Tick marks represent censored patients - Lee et al. 2021
Persistent HHV-6 by D+100 was associated with nearly three-fold increased mortality (adjusted hazard ratio, 2.97; 95% CI, 1.62-5.47; p=0.0005), after adjusting for age, antiviral treatment, and absolute lymphocyte count.
Reinforcing the high risk of HHV-6 infection in those being treated for serious hematological conditions, a second study by Gonzalez et al. (2021) from the Institut Paoli-Calmettes in Marseilles, France, performed a retrospective study on all consecutive adult patients with hematologic malignancies admitted to a single comprehensive cancer center ICU over a 6 year period. RT-PCR was used to detect viral DNA detected by in blood, pulmonary samples, cerebrospinal fluid, urine, other fluids and tissue samples. Information on patient outcomes was systematically collected.

Summarized virus detection data Gonzalez et al. 2021
The viral DNA detected most often (18% of subjects) was HHV-6. Multivariable analysis that adjusted for other mortality risk factors found that the detection of HHV-6 DNA independently increased the odds of hospital mortality over two-fold (OR: 2.35 95% CI, 1.03-5.34; P=0.042). HHV-6 pneumonitis was independently found to increase the risk of 1-year mortality by 6.87x (Odds ratio 95% CI, 1.09-43.3; P=0.04). Antiviral prophylaxis during ICU stays decreased odds of hospital mortality rates by half (Odds ratio 0.41 95% CI 0.18-0.95; P=0.037), in this observational study.
Thus, this study finds that detecting HHV-6 DNA in various body samples is associated with increased hospital mortality, and that HHV-6 pneumonitis is associated with increased one-year mortality. Particularly since treatment was not randomized in this study, it cannot be concluded that HHV-6 directly causes increased mortality, as contrasted to being a marker for other unmeasured factors that increase mortality.
Future randomized control studies utilizing antivirals against HHV-6 seems like the next logical step to further assess the impact of HHV-6 on mortality.
Read the full articles: Gonzalez 2021 & Lee et al. 2021