Patients with low levels of HHV-6 antibodies might benefit from treatment from IVIG or novel neutralizing antibodies before cord blood transplantation.
HHV-6B reactivation often occurs following hematopoietic stem cell transplantation (HSCT), particularly following the use of cord blood. Following and preceding HSCT, Nakayama et al of Keio University School of Medicine measured levels of anti-HHV-6 IgG antibodies in 56 consecutive adult HSCT patients, receiving allogeneic grafts of different types.
Consistent with previous studies, multivariate analysis revealed that cord blood transplantation (CBT) was an independent risk factor for HHV-6 reactivation (OR 8.6 (2.3-32.6) P<0.01). The investigators then looked at risk factors for HHV-6 reactivation in the CBT cases. As expected, all but one of these adult patients was seropositive for HHV-6. However, the anti-HHV-6 antibody levels were significantly lower in CBT patients with HHV-6 reactivation compared to those without HHV-6 reactivation, consistent with previous work, including from these authors (Yamane et al 2007.)
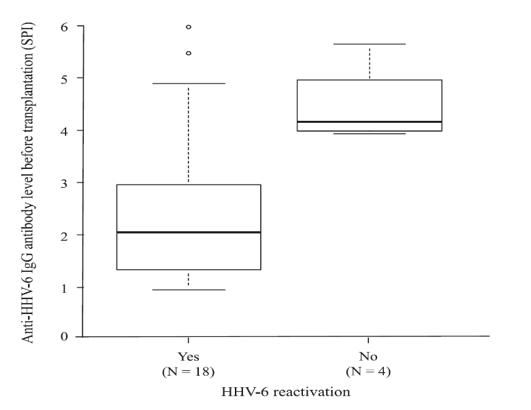
Figure 1 - IgG antibody levels in adult cord blood HSCT recipients that experience reactivation of HHV-6 or not (Nakayama et al. 2020)
The team performed the serologic studies using both immunofluorescence assay (IFA) and enzyme-linked immunosorbent assay (ELISA), and found that the results of the two assays were significantly correlated (r = 0.53, P<0.01).
These results suggest that lower natural levels of IgG to HHV-6 may be a risk factor for HHV-6 reactivation in adults undergoing HSCT with cord blood. If so, theoretically it could be useful to measure anti-HHV-6-IgG antibody levels prior to transplantation, and to treat patients who have low levels with novel neutralizing antibodies or immunoglobulin.
Read the full article: Nakayama 2020

