A team from the University of Washington conducted a retrospective observational study using a large U.S. open source database containing detailed records of patients undergoing alloHSCT from 2012-2017. The database recorded the presence and number of dsDNA viral infections that were detected within 1 year after alloHSCT and the associated expenses of performing the transplant and dealing with any complications and hospital readmissions, as well as the outcomes. The team studied patients infected with cytomegalovirus (CMV), BK virus, Epstein-Barr virus (EBV), JC virus, adenovirus (ADV) and HHV-6.
The primary findings from the study were:
- 30% were diagnosed with single infections and 10% were diagnosed with two or more infections.
- The length of hospital stay increased with each additional reactivated virus, from 41 days in patients with no viral infection to 61 days with one viral infection and 103 days for three or more infections.
- Viral reactivation was associated with significantly increased financial burden: a single viral infection increased the cost of care to $431,614 compared to $266,345 for patients with no viral infection. The cost for patients with two viral reactivations was higher at $639,097 and the expense rose to $964,378 for patients with three viral infections.
- A greater proportion of patients developed renal impairment after diagnosis of first dsDNA virus (18.3%, n=962) compared with those who developed renal impairment before diagnosis of dsDNA infection (9.2%, n=481)
- As shown in Figure 1, all-cause mortality also increased with reactivation, and was greatest in those the more viruses reactivated, regardless of whether graft-versus-host disease was present or not.
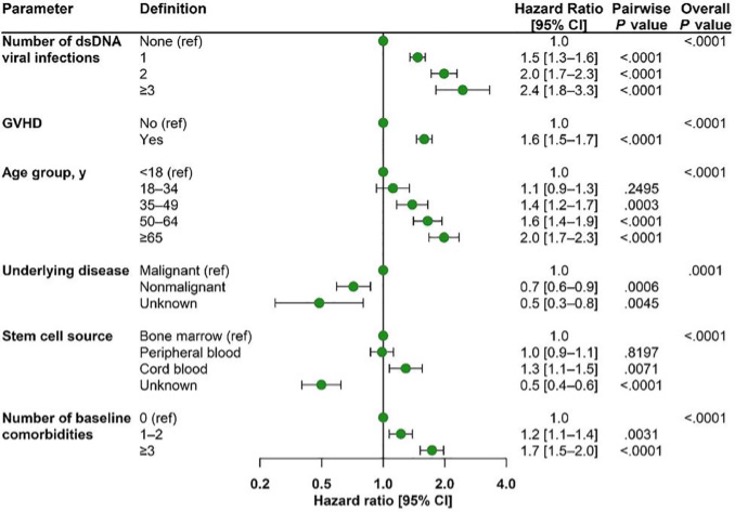
Figure 1. Adjusted Cox proportional hazards model for time to all cause mortality for multiple dsDNA viral infections, adjusted for GVHD during follow-up, age, underlying disease, stem cell source, and number of comorbidities.
The studies gathered in this retrospective observational database did not systematically look for all possible reactivated viruses, and thus the relative prevalence of different viruses reported is not particularly meaningful. While most institutions routinely test for CMV, HHV-6 is typically only tested when the patient develops neurological symptoms. As a result, there were 3,878 CMV infections recorded, but only 561 for HHV-6. When systematic testing has been done for HHV-6, the reactivation rate is far higher.
This analysis does make it clear that reactivation of dsDNA viruses during alloHSCT is associated with much worse outcomes, and much greater expense.
The study design does not allow a determination of whether: 1) the viral reactivation causes the worse outcomes and greater expense or whether 2) patients with viral reactivation may be inherently sicker, leading to the worse outcomes and greater expense. Yet since the first possibility is plausible, the study underlines the importance of developing improved technologies and strategies for preventing, diagnosing and treating reactivated viral infections in people undergoing alloHSCT.
Read the full article: Hill 2022

