The complications from reactivated CMV infection in post-hematopoetic cell transplant (HCT) period are well recognized. But non-CMV herpesvirus (NCHV) infection can also cause complications and is associated with increased mortality after HCT (Servais 2014; Gonzalez 2021; Lee et al. 2021).
In the largest retrospective study comparing incidence and outcomes of NCHV infections, Singh et al. (2021) of the University of Kansas Cancer Center aimed to evaluate the incidence of reactivated infection with non-CMV herpesviruses in 2765 patients receiving post-transplantation cyclophosphamide (PTCy) to reduce the risk of graft-versus-host disease (GVHD), as stored in a large multi-institutional database.
The database contained three groups: haploidentical transplant with PTCy (HaploCy, n=757), matched sibling donor transplants with PTCy (SibCy, n=1605), or matched sibling donor transplant with calcineurin inhibitor-based prophylaxis (SibCNI, n=403). The cumulative incidence of NCHV infection at six months post-transplant in HaploCy, SibCy, and SibCNI were 13.9% (99%CI=10.8-17.3%), 10.7% (99%CI=7.1-15%), and 5.7% (99%CI=4.3-7.3%), respectively. As with CMV, HaploCy had higher rates of infection.
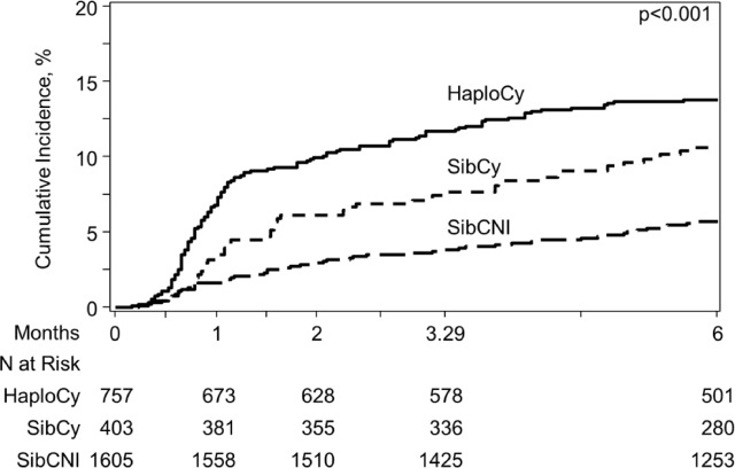
Cumulative incidence of NCHV at various time points.
HHV-6 contributed to the majority of NCHV in both HaploCy and SibCy arms [HaploCy = 9.3%; SibCy = 5.7%; SibCNI = 1.9%].
Patients who developed NCHV—particularly HHV-6 reactivation—within 40 days of transplantation had higher treatment-related mortality, particularly in the HaploCy group. Given the retrospective nature of the study, no causal inferences are possible.
A strength of the study is its large size and multi-institutional dataset. Limitations are its retrospective and observational nature; lack of control over the techniques used at the various institutions to detect NCHV, and over when to deploy those techniques; and failure to distinguish HHV-6A from HHV-6B (although the latter likely was predominant). Another limitation is the failure to distinguish people with iciHHV-6, who might have been scored as having reactivated infection on the basis of viral load studies.
Overall, this study demonstrates that PTCy is associated with an increased risk of NCHV infection, primarily manifested as HHV-6 viremia, which was then associated with increased mortality, especially in the HaploCY cohort. These findings justify more controlled prospective studies of non-CMV herpesvirus infection—particularly HHV-6—in the post-HCT setting.
Read the full article: Singh 2021

