Those with the highest viral loads suffered deficits in verbal memory and reduced quality of life.
A Japanese multi-center study, led by oncologist Masao Ogata of Oita University and the Japan Society for Hematopoietic Cell Transplantation, reports confirmatory evidence of cognitive deficits in people with reactivation of HHV-6B during cord blood HCT. The team found that 19% of patients developed delirium, and that the reactivation of HHV-6B preceded delirium in 86% of those cases, with median lag of 7 days. Older age (>55) was the only risk factor identified for HHV-6B associated delirium.
In a memory test of word recall, those with HHV-6B reactivation saw their scores reduced 31%. Moreover, patients with the highest level of HHV-6B reactivation saw their scores reduced by greater than 40%. Quality of life (QOL) was assessed using a validated and widely-used instrument (the 36-item Short-Form Health Survey). The social functioning score one year post-transplantation was significantly lower in older patients (>55) and in those who experienced higher-level HHV-6B reactivation than in those who did not.
Prior research from the U.S. has found that delirium and new cognitive deficits (including attention, processing speed and concentration) can occur in patients who have reactivation of HHV-6B during hematopoietic cell transplantation (HCT), particularly in those with HHV-6B encephalitis (Zerr 2011; Hill 2015) and that this may be mitigated by antiviral therapy (Hill 2015). Reactivation of HHV-6B occurs in many patients undergoing all forms of HCT, and in up to 90% of patients undergoing cord blood transplantation. Encephalitis due to HHV-6B occurs in about 1% of all types of HCT, but in up to 8-10% of people following cord blood HCT.
Investigators studied 45 patients aged 16 or greater had cord blood HCT over a three-year period. Of these 45, 37 underwent all the virologic and neurologic testing required by the study. Of the 37, 7 (19%) developed delirium, lasting about a week after developing HHV-6 viremia.
Blood was obtained twice a week through day 70 post-HCT, and the HHV-6 DNA load measured. The median peak plasma HHV-6 DNA load was 16,134 copies/ml (range, less than the detection limit to 270,800 copies/ml). As a result, the investigators set the threshold for “higher-level HHV-6B reactivation” at plasma HHV-6 DNA loads of ≥ 16,134 copies/ml. Consequently, half of the 37 patients were found to have relatively high viral loads.
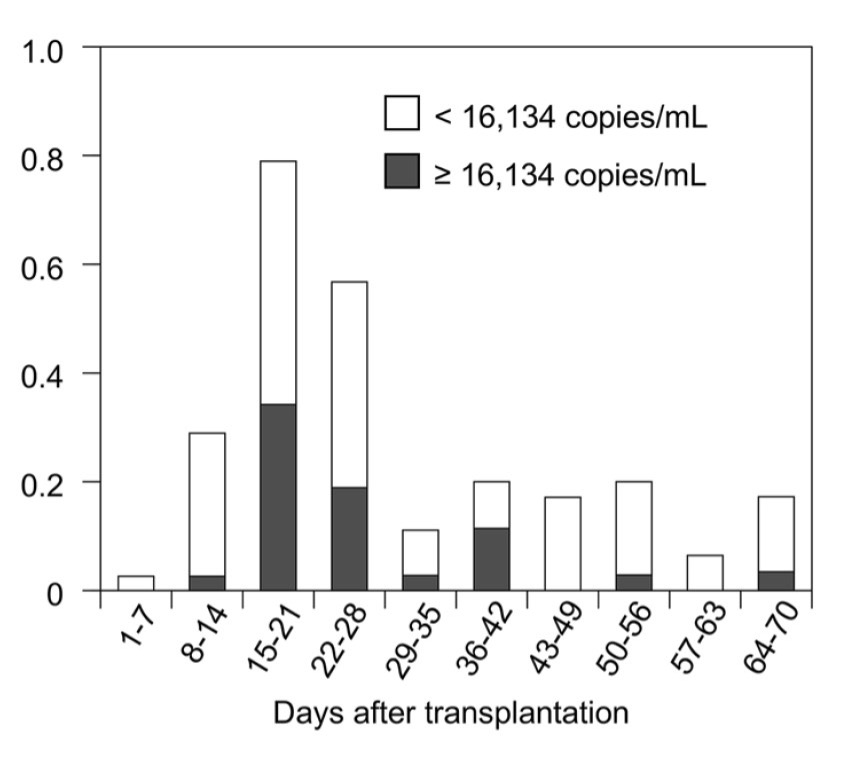
Figure 1. Proportion of patients with positive HHV-6 DNA results in each post-transplantation period.
The timing of reactivation is shown in Figure 1.
Objective testing of verbal memory before vs. after HCT found a statistically significant drop in verbal memory (P = 0.004) among those patients who experienced higher-level HHV-6B reactivation. Patients with no reactivation, or lower viral loads, did not experience significant declines in verbal memory scores. Various possible confounding factors—age, gender, disease status at the time of the HCT, conditioning regimens, total body irradiation, development of acute graft-versus-host disease—did not correlate with the development of cognitive impairment: of the variables measured, only the higher levels of HHV-6B reactivation correlated with cognitive impairment. The change in verbal memory scores from before vs. after HCT, in those without high levels of HHV-6B reactivation vs. those with high levels, is shown in Figure 2.
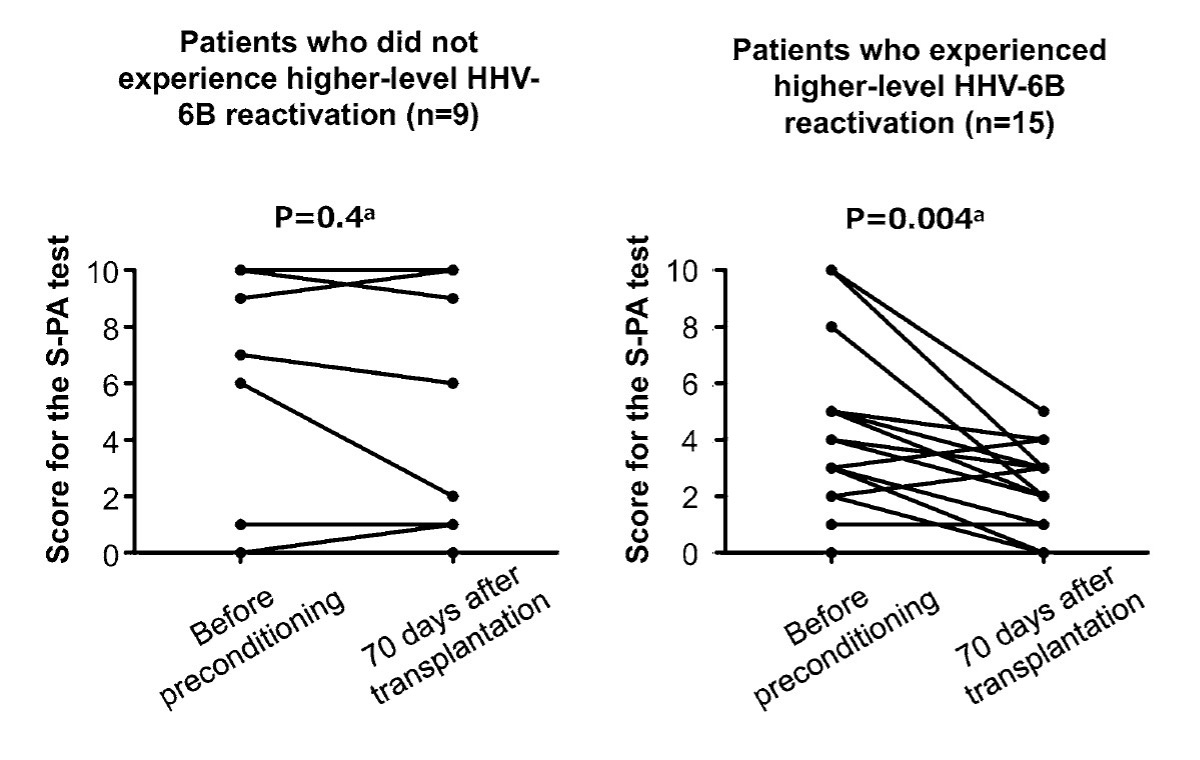
Figure 2. Score for verbal memory test (S-PA test), with higher scores indicating better memory, in those without and with higher-level HHV-6B reactivation.
In contrast to previous studies, deficits in attention and processing speed were not identified in these patients.
The reason that social functioning was impaired was not pursued, but it is plausible that cognitive impairment contributed to reduced interest in, or ability to engage in, social activities.
This study from Japan, studying exclusively cord blood HCT, comes to similar conclusions as previous studies from the U.S. studying primarily allogeneic bone marrow HCT: high-levels of HHV-6B reactivation following HCT are correlated with the development of delirium and with persisting cognitive deficits. While there are some differences in the type of cognitive deficits experienced, these differences may reflect differences in the tests used, the type of blood cell transplant, and the relatively small size of the studies.
Read the full article: Ogata 2024