T-cell responses correlate directly with clinical symptoms, and were better predictors of HHV-6 disease than viral load or total CD3+ counts.
Identifying patients at risk of HHV-6 is difficult because viral loads can change rapidly. A team from the Ospedale San Raffaele Scientific Institute in Milan evaluated the clinical utility of using an ELISpot assay to identify patients at risk of developing severe symptoms by assessing HHV-6-specific T cell responses.
The team prospectively followed 208 alloHSCT patients who were prospectively monitored weekly for HHV-6 reactivation with real-time quantitative PCR, and monitored regularly for HHV-6 related complications. Patients with iciHHV6 were excluded.
The most interesting findings of this study were as follows:
- HHV-6-specific T cell responses were quantified at >4 days after the first viremia detection—predicted clinically relevant infections (P < .0001), with higher specificity (93%) and sensitivity (79%) than did quantifying polyclonal CD3+ cells (Figure 1).
- Approximately 90% of patients who reactivated with HHV-6 could be screened successfully for HHV-6-specific immune response.
- HHV-6 reactivation occurred in 63% of patients; the median time to HHV-6 reactivation was 25 days (range 3-538 days)
- Circulating HHV-6-specific T cells were significantly higher in patients with reactivated virus.
- HHV-6 reactivation was not significantly associated with transplant-related mortality or overall survival (although the power of the study to recognize such associations as being significant was poor).
- As with previous studies (Phan 2018), HHV-6 reactivation was significantly associated with risk of acute GVHD.
- HHV-6-related complications included delayed engraftment or myelosuppression (n = 39) and proven encephalitis (n = 4), with a concomitant syndrome of inappropriate antidiuretic hormone secretion (SIADH) in 1 case.
- As was shown by the same group previously (Greco 2016) higher CD3+ cell counts protected against HHV-6 reactivation, as shown in Figure 1.
- No deaths clearly related to HHV-6 infection were reported. In contrast, there were 53 deaths due to disease relapse and 51 due to transplant-related mortality.
- Multivariable analysis identified the following risk factors for HHV-6 reactivation: previous allo-HSCT, posttransplant cyclophosphamide (PT-Cy), and treatment with steroids.
- There was no cross-reactivity or association between CMV and HHV-6 responses.
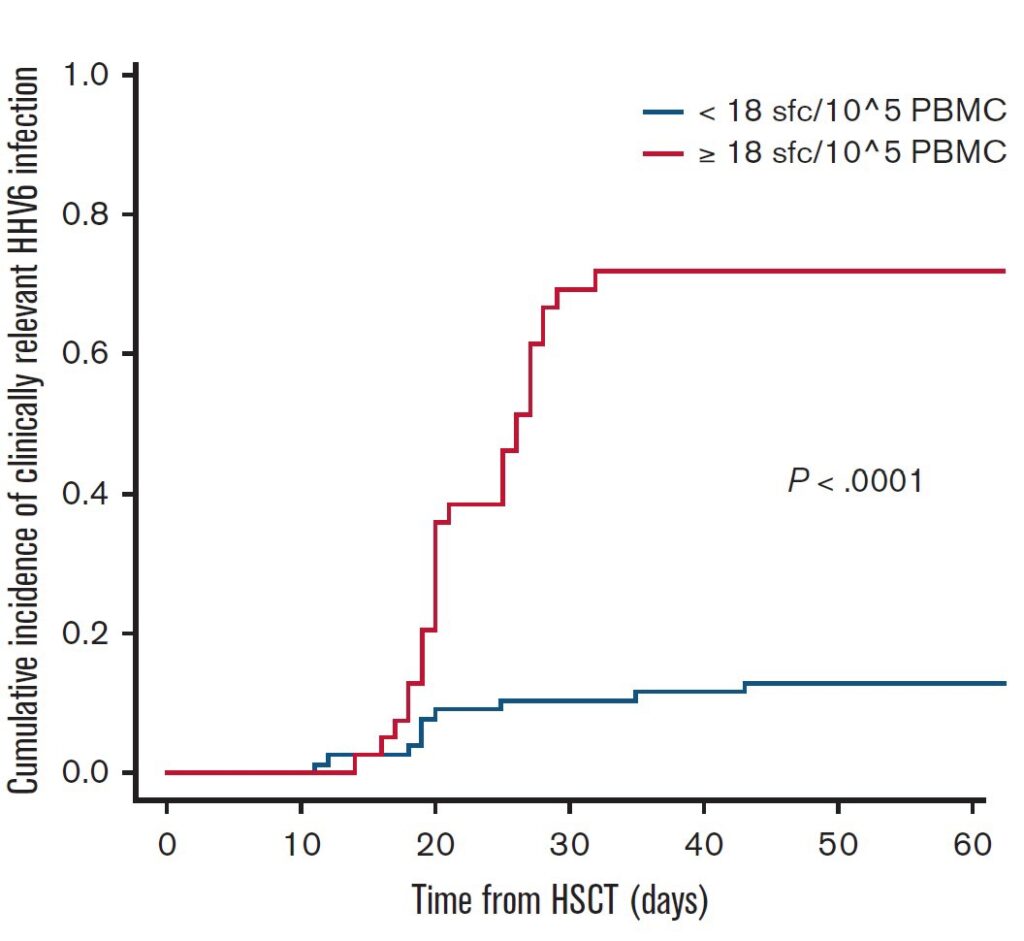
Figure 1. Cumulative incidence of clinically relevant HHV-6 reactivations in people with different numbers of HHV-6–specific spot forming cells (SFC)/105 PBMC (above the threshold of 18, in blue, and below the threshold in red).
Of interest, the results with HHV-6-specific T cell responses is quite different from the experience with CMV-specific T-cell responses and disease; high levels of CMV-specific T cell responses via ELISpot indicate protection from disease and lower rates of reactivation. The authors speculate that the relatively low frequency of HHV-6 specific T-cells may be related to the lymphotropism of the virus or to its immunosuppressive properties (Becerra 2014).
This prospective study again supports an important association of HHV-6 reactivation with acute GVHD. While it does not find convincing evidence of an association of HHV-6 reactivation with transplant-related mortality or overall survival, the study was underpowered to recognize such associations as statistically significant. Finally, the study reinforces the importance of HHV-6-specific T cell responses in protecting against HHV-6-related clinical complications.
Read the full article: Noviello 2023

