Steroids reduced cardiac inflammation in 70% and improved ejection fraction in 80% without an increase in viral load.
HHV-6 causes myocarditis in children with primary infections (Reddy 2017) and previous work from Charité University Hospital in Berlin has found HHV-6 DNA in endomyocardial biopsy (EMB) heart tissue from people with unexplained heart failure who are not improving with conservative therapy (Kuhl 2005, Mahrholdt 2006).
In cases of lymphocytic myocarditis, the inflammation is typically treated by immunosuppressive medications. However, the European Society of Cardiology guidelines state that immunosuppression should not be administered in patients with viral infections since such treatment also may trigger reactivation of latent viruses, with adverse clinical consequences. Patients with high levels of viral DNA in EMBs and associated inflammation are generally assumed to have a viral myocarditis that can lead to heart failure and are treated with antimicrobials instead of immunosuppression.
To examine this risk-benefit trade-off in cases of moderately positive HHV-6 infection, the investigators determined the clinical outcome in 10 patients with symptomatic heart failure and HHV-6 DNA in myocardial tissue who were given an immunosuppressive regimen of prednisolone and azathioprine. This treatment was given at physician discretion, not as part of a controlled study. The patients were selected from over 756 patients with unexplained heart failure who failed conservative therapy and underwent endomyocardial biopsy (see Figure 1). Approximately 15% of the lymphocytic myocarditis patients were HHV-6 DNA positive. Repeat EMBs were performed to look for objective evidence of benefit.
In the ten patients that received immunosuppressive treatment, there was improvement in symptoms (New York Heart Association class), as well as objective markers: the grade of inflammation on repeat biopsy, left ventricular ejection fraction rose from 41.9 to 49,9, end-diastolic diameter of left ventricle fell, and levels of NT-proBNP (a blood marker of heart failure) were reduced from 623 to 80. HHV-6 copy number in blood went down in most patients but up in a few. However, no cases of disease caused by HHV-6 reactivation were reported.
In a second study, the investigators examined 26 patients with low levels of viral DNA in biopsy specimens – detectable by nested PCR but at a viral load too low to quantify by by real-time PCR (eg <100 copies of HHV-6 DNA/μG of cardiac DNA).
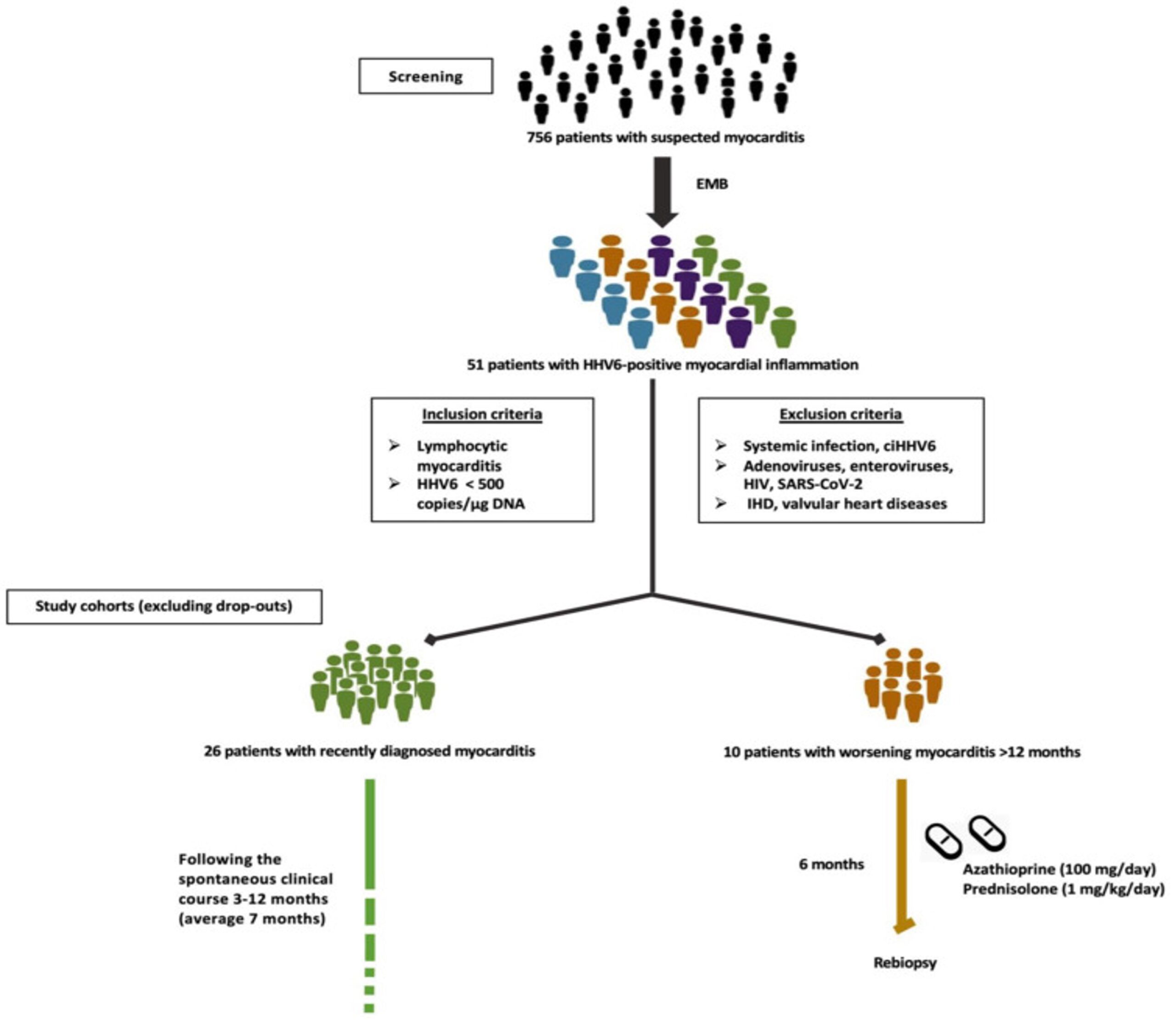
Figure – Study design
In these 26 people with recent-onset untreated lymphocytic myocarditis confirmed by EMB, and who had low levels of viral DNA, over an average of seven months of follow-up, 60% of people experienced improvement in symptoms and cardiac function (left ventricular ejection fraction). Thus, regardless of whether the viruses were the cause of the lymphocytic myocarditis, the short-term outcome in such patients was relatively good.
In comparing patients who were positive vs. negative for HHV-6 DNA in EMBs, they noted no significant difference in the two groups with regards to the expression of NLRP3 inflammasome pathway genes or protein levels of cardiac remodeling markers (by mass spectroscopy), raising a question as to whether the virus present in cardiac tissue really was provoking pathology.
The uncontrolled treatment results suggest that the benefits of immunosuppressive treatment in such patients may outweigh the risks, but controlled studies are necessary to draw firm conclusions.
The study of people with low levels of viral DNA in EMB raise questions about the pathogenic role of low level virus in these patients, and suggest that they may have a relatively positive natural improvement in symptoms and cardiac function.
Read the full article: Elsanhoury 2022