Chinese investigators determined that human leukocyte antigen polymorphism HLA-B*13:01 and HHV-6 DNA positivity in blood both were not only independently associated with occupational trichloroethylene hypersensitivity, but they also had an interactive effect, increasing the odds ratio to 92.
Occupational trichloroethylene hypersensitivity syndrome (OTHS) is a drug-induced hypersensitivity syndrome that afflicts workers exposed to trichloroethylene, a widely used solvent and degreasing agent. OTHS results in a syndrome similar to drug reaction with eosinophilia and systemic symptoms (DRESS) or drug- induced hypersensitivity syndrome (DIHS). It has a high mortality rate with about 7% of patients dying of organ failure. It is considered to be a T cell-mediated Type IV hypersensitivity reaction as the latency is about 2-5 weeks, and the reaction is systemic rather than being limited to the area of contact.
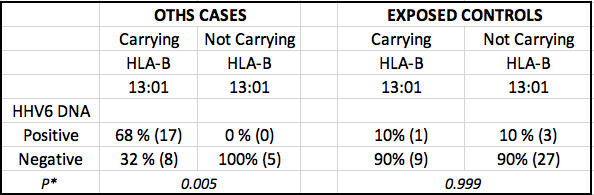
69% of the OTHS cases carrying the allele were positive for HHV-6 DNA, compared to 0% of cases without the allele. In exposed controls 10% were positive for HHV-6B DNA in whole blood, and there was no difference between carriers and non-carriers of the allele.
A Chinese study compared 30 patients with OTHS and 40 controls who were exposed to trichloroethylene but did not develop hypersensitivity. Carrying HLA-B*13:01 resulted in an OR of 9.17 (p=.001) and carrying HHV-6 DNA in whole blood resulted in an OR of 5.7 (p=.015), but carrying both resulted in an OR of 91.8 (p=0.001). There was no impact from CMV DNA positivity.
Of interest, among the OTHS cases, 68% of the HLA-B*13:01 carriers were positive for HHV-6 DNA, vs 0% of the OTHS cases negative for the polymorphism.
There was no difference in the rate of HHV-6 DNA positivity in whole blood samples between controls with and without the HLA-B*13:01 allele. The rate of CMV DNA detection in OTHS cases (30%) was higher than that of controls (15%), but it was not statistically significant.
HLA-B*13:01 has also been found to play a role in dapsone hypersensitivity cases (Zhang 2013), with an odds ratio of 20.5 and a specificity as a predictor of 86%.
A previous study found HLA-B*1301 in 74% of 113 OTHS cases, compared to 9.2% of tolerant controls (Li 2007).
The association of type IV reactions with HLA alleles has led to HLA-allele-specific screening for the prevention of drug hypersensitivities, including HLA-B∗57:01 screening to prevent abacavir hypersensitivity reaction, and HLA-B∗15:02 screening to prevent carbamazepine-associated Stevens-Johnson syndrome/toxic epidermal necrolysis, mostly in Asian populations.
Timeline of class I and II HLA associations and drug hypersensitivity.
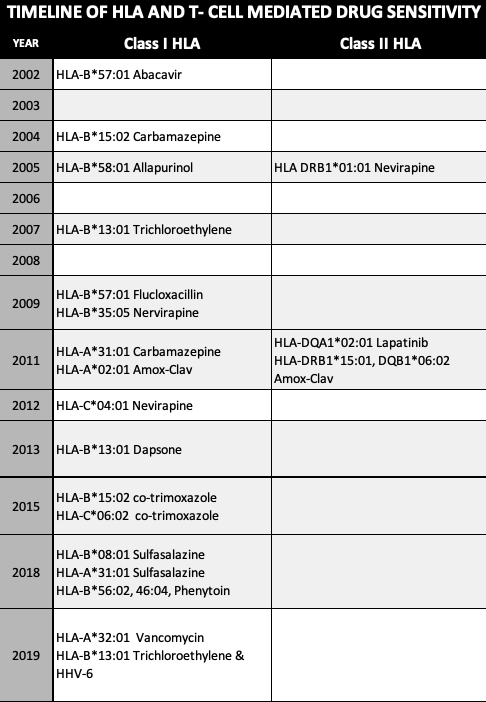
Timeline of class I and II HLA associations and drug hypersensitivity.
Man-made small molecules and/or their metabolites can interact with HLAs to result in dangerous T cell–mediated hypersensitivity syndromes. It has already been demonstrated that pre-existing class I–restricted effector memory T cell responses to common herpesvirus infections can mediate organ rejection (Pavlos 2015).
In drug hypersensitivity, memory T cells that are specific for a herpesvirus peptide might cross-react with an endogenous peptide by several possible mechanisms. According to the “heterologous immunity” model, the memory T cells are generated after viral exposure and reside at specific sites, depending on the pathogens involved. These memory T cells can then be activated by interactions between the culprit drug and endogenous “self” peptides, or they can be directly activated by drug binding to an immune receptor in a pharmacological interaction (Pavlos 2015) (White 2015).
In 2014, Japanese investigators found a very strong relationship between HLA-B*40:06 and HHV-6 encephalopathy/encephalitis post-stem cell transplant. HLA mismatch conferred an increased risk of only 4.5X while the presence of HLA-B*40:06 resulted in an impressive OR of 31.1 (p=0.027) (Yamamoto 2014). HLA alleles have also been identified as risk factors for ocular Behcet’s disease and Rasmussen’s encephalitis.
To read the full paper, click here: Wang 2019.

Models explaining hypersensitivity syndrome. (a) Models of T cell activation. Viral peptide A is selectively bound to the MHC and presented by the APC to activate T cells through the TCR. Peptide B is unable to bind the MHC and is excluded from the repertoire of ligands presented in the context of this MHC allotype. (b) Heterologous immunity model. Memory T cells are generated after virus or other pathogen exposure and reside at specific tissue sites. These memory T cells cross-react with an altered repertoire of endogenous peptides after trichloroethylene, or its metabolites, bind to the MHC. Source: Wang 2019, International Archives of Occupational and Environmental Health.
Team from the Shenzhen Prevention and Treatment Center for Occupational Diseases in Shenzhen, China. In the first row, from left to right, Dafeng Lin (the corresponding author), Yanfang Zhang (Department Dean), Dianpeng Wang (the first author)