HHV-6 reactivation in both skin and blood was found frequently in severe cases
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) is a rare but severe adverse event following the administration of certain pharmaceuticals. DRESS is triggered by the administration of certain drugs—most often allopurinol, antiepileptic drugs (e.g. carbamazepine, phenytoin) and sulfonamides (sulfasalazine, trimethoprim-sulfamethoxazole).
The illness begins typically beginning about 2-8 weeks after the drug is given. It is manifested by a diffuse maculopapular rash, swelling of the face, enlargement of lymph nodes, fever and increased numbers of circulating eosinophils and/or atypical lymphocytes. In severe cases, damage to the liver, kidney, pancreas, lung, heart, skeletal muscle can occur, as can meningoencephalitis. In most series, the mortality rate is around 10%.
Past studies have found frequent reactivation of several herpesviruses, including HHV-6, in peripheral mononuclear cells. Indeed, in Japan, the detection of reactivated HHV-6 is included in the diagnostic criteria for DIHS. Although HHV-6 reactivates in a high proportion of people with DRESS, it reactivated far less often in other cutaneous drug reactions such as Stevens Johnson Syndrome (SJS) or toxic epidermal necrosis (TEN). Few studies of HHV-6 reactivation in skin biopsies have been performed.
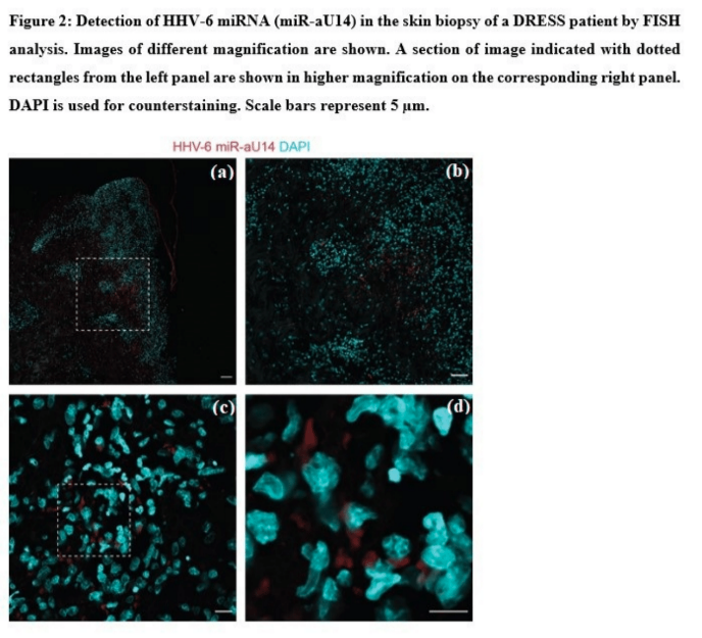
A multi-center team from five university hospitals in France gathered data from 2007 to 2021 on 52 patients with severe DRESS: eight patients died (15%), 13 (27%) were admitted to ICU, and 34 (65%) had multiorgan injury. To assess the presence of reactivated virus in formalin-fixed, paraffin-embedded skin biopsies, the team measured the small non-coding transcript of HHV-6, miR-aU14 (Prusty 2018, Hennig 2022), and late viral protein GP82/105.
The drugs that most frequently triggered DRESS in this case series were allopurinol (n = 21; 40%), carbamazepine (N = 6; 12%) and sulfasalazine (n = 5; 10%).
Reactivation of HHV-6, EBV or CMV in the blood was demonstrated in 40 patients (77%); reactivation of two of these viruses was seen in 21 (53%); reactivation of HHV-6 was seen in 26 (50%) of patients, of EBV was seen in 56% and of CMV was seen in 21% of patients.
Reactivation of HHV-6 in skin biopsies was seen in in 15/20 (75%) of the patients from whom biopsies were obtained. In these 15 patients with reactivated HHV-6 in the skin, 83% also had reactivation in the blood. The median time between drug administration and reactivation of HHV-6 in the blood was 24 days; in skin it was 11 days. Of those who were positive for HHV-6 in blood by PCR, reactivation in the skin was detected in 10/12 patients. The two biomarkers of reactivation correlated strongly; for example, no patient had GP82/105 positivity without also having positivity of miR-aU14.
Histologic studies found that reactivated HHV-6 was present in the inflammatory cells infiltrating the dermis of the skin, and occasionally also in sweat glands. The specific inflammatory cell types in which HHV-6 was reactivated were not identified. In contrast, in skin biopsy specimens from 15 patients with inflammatory skin diseases other than DRESS, HHV-6 reactivation was never seen in the dermis, though it was occasionally seen in sweat glands.
As for the types of inflammatory cells in the skin that harbor virus, previous studies have reported that in DRESS both monocyte and myeloid cells in skin harbor reactivated virus, and may pass the virus on to CD4+ T cells (Hashizume 2013).
In recent years, most severe drug allergies have been associated with specific HLA alleles (Gibson 2023). For example, allopurinol sensitivity is associated with HLA-B*58:01 and carbamazepine is associated with HLA-B*15:11. However, the mechanisms by which DRESS leads to reactivation of herpesviruses, particularly HHV-6, remain uncertain.
The authors note two theories on why HHV-6 reactivates in DRESS (1) immunosuppression at the outset of DRESS (mediated by unclear mechanisms) and (2) the possibility that the drug itself might trigger reactivation of herpesviruses.
Several in vitro studies have found that allopurinol and carbamazepine both can reactivate latent HHV-6 in cell culture. They may encourage reactivation by inducing epigenetic changes—particularly histone deacetylation and DNA methylation. That hypothesis is plausible because some of the drugs that trigger DRESS—particularly carbamazepine and valproic acid—induce such changes, and because histone deacetylase inhibitors like trichostatin also induce reactivation, in vitro. In addition, differences in methylation profiles have been identified between patients who developed allopurinol-induced DRESS and those who did not (Sun 2018).
One wishes that instead of being a case series this study was a prospective observational study in which the clinical and biological data was obtained repeatedly at specific times, according to protocol. However, such studies are very hard to organize and fund when the disease is rare. And since this study involved patients who are even more rare—those very severely ill—organizing a prospective observational study would have been very difficult. Nevertheless, this excellent case series study supports a role for reactivation of HHV-6 from white blood cells, and possibly from harbors in the skin, in DRESS.
Read the full article: Marcombes 2023

