C. trachomatis infection activates latent HHV-6, and HHV-6 in turn promotes persistence of C. trachomatis. Both have been reported in cases of ovarian cancer, leaving the authors to wonder if a co-infection might increase the risk for developing ovarian cancer
HHV-6 is not recognized as a causative agent for cancer, but a microarray study of the ovarian cancer microbiome done in 2017 showed HHV-6A sequences more frequently in ovarian cancer tissues than in control tissues, including 10% of cases showing HHV-6 integration (Banerjee 2017). Chlamydia trachomatis is a bacterium that can cause DNA damage and inhibit the host cell’s DNA repair system, resulting in genomic instability and potentially oncogenic mutations.
Researchers Nitish Gulve and Thomas Rudel from the University of Wuerzburg in Germany reviewed the interaction of C. trachomatis and HHV-6 in the development and progression of ovarian cancer and suggest that C. trachomatis infection may create an environment that is conducive for the integration of viral sequences of HHV-6 known as direct repeats (DRs) into host DNA. The presence of these DRs, they speculate, can disrupt host cell functions and exacerbate genomic instability.
HHV-6A has also been found in the uterus of a subset of >30% of women with unexplained infertility, but in none of the controls (Marci 2016; Coulam 2018). Women experiencing infertility also have an increased risk for ovarian cancer. Since HHV-6B is the most common strain to reactivate in transplant patients, it is striking that HHV-6A (and not HHV-6B) was found in both the uterus and ovarian cancer tumors.
Antibodies to immediate early proteins of HHV-6A were also found to be a significant risk factor for non-Hodgkin’s lymphoma (Bassig 2018). The possible role of HHV-6 in malignancy has recently been reviewed (Eliassen 2019).
The authors conclude that it is “time to strip HHV-6 off its ‘benign’ label and consider its coinfection with C. trachomatis and/ or other pathogens for further in-depth studies.”
Read the full text: Gulve 2019
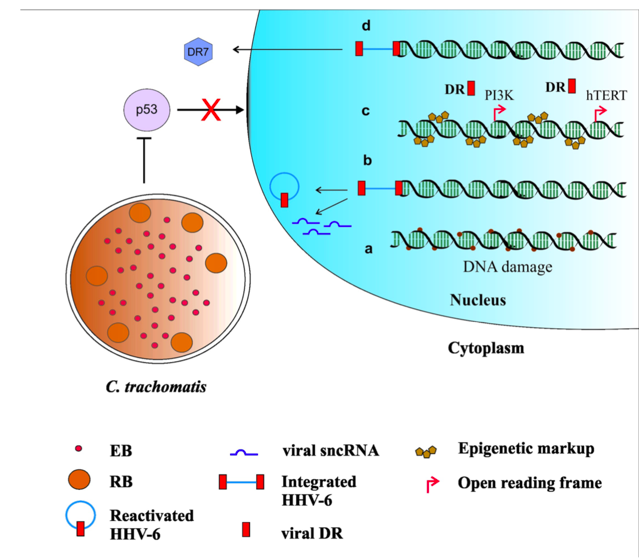
Consequences of C. trachomatis and HHV-6 co-infection.

