
Elizabetta Caselli, PhD (center) and co-workers at University of Ferrara, Modena, Italy
A group led by Elisabetta Caselli, PhD, at University of Ferrara showed HHV-6A in the skin and elevated HHV6-B DNA in the peripheral blood of systemic sclerosis patients.
Systemic sclerosis (SSc) is an uncommon, devastating and incurable autoimmune disease characterized by vascular obliteration, immunological abnormalities, and excessive extracellular matrix deposition, which causes fibrosis of the skin and internal organs. The disease is believed to be a multifactorial process involving both genetic and environmental factors, among which HHV-6 infection was first suggested as a possible trigger over a decade ago (Broccolo 2009).
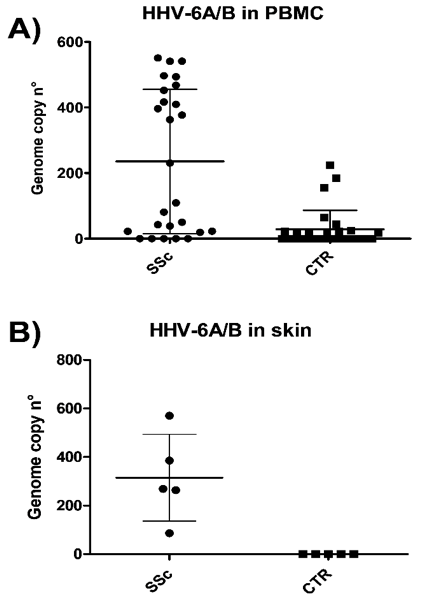
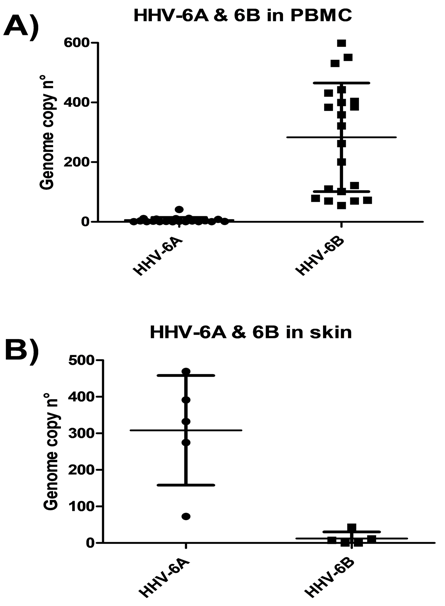
Caselli's group found a significantly higher prevalence of HHV-6A/6B DNA in the blood and skin tissue of SSc patients compared to controls (p < 0.0001). Of note, all SSc skin biopsies were positive for HHV-6A DNA, whereas no samples derived from healthy skin harbored HHV-6A/B (p < 0.005). Although HHV-6A was prominent in the tissues, HHV-6B was dominant in the blood.
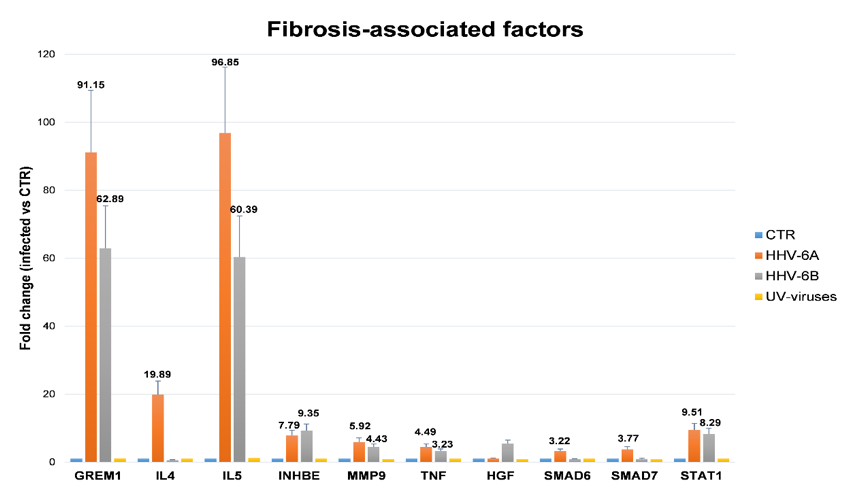
Importantly, higher virus loads correlated with SSc severity, as well as the prevalence and titer of antibodies directed against HHV-6 U94, and the impairment of NK response against the virus, which was particularly evident in patients expressing KIR2DL2 receptors, supporting previous observations by the group (Caselli 2006). In addition, as a proof of concept, they showed that HHV-6 infection in vitro can induce the expression of pro-fibrotic molecules in endothelial cells.
Caselli’s group had previously reported that HHV-6A infection is associated with the development of autoimmune thyroiditis, a condition which frequently precedes the development of multi-organ pathology in SSc patients (Caselli 2012), and that HHV-6 infection inhibits the angiogenic properties of endothelial cells, whose injury represents one of the first steps in the pathogenesis of SSc (Caruso 2009).
A recent study has also found elevated antibodies to Epstein Barr virus (Efthymiou 2018). And another study found SSc patients to have elevated antibodies to H. pylori, CMV, EBV, and parvovirus B19 compared to controls (Bilgin 2015). The authors hope that their findings on HHV-6A/B in SSc will encourage future studies to confirm their data and clarify the mechanisms by which viral infection might ultimately favor SSc development.
See the full paper: Caselli 2019

