At the height of the COVID-19 pandemic, a 59-year old man was admitted to a hospital in Italy with fever and breathlessness. Labs showed elevated CRP, leukocytosis, dramatically elevated liver enzymes, bilirubin, and cardiac troponin. His chest CT showed ground glass opacities. His echocardiogram revealed pericardial effusion with normal heart pumping function (ejection fraction of 60) and his ECG demonstrated sinus tachycardia. In short, the man appeared to have systemic disease involving the heart, lung and liver.
Infection with SARS-CoV-2 was suspected. However, PCR testing of nasopharyngeal swabs was negative twice. The patient’s condition worsened on the third day, and he died of a sudden cardiac arrest.
Whole body autopsy revealed pleural and pericardial effusions, consolidation of lung tissue and lymphocytic infiltrations in many organs (including lungs, liver and skeletal muscle).
As shown, in part, in the figure below, the heart was enlarged, the walls of the ventricles were thickened, the endocardium revealed frequent punctate petechial hemorrhages and the coronary arteries had an inflammatory infiltrate in the intima and media. The heart muscle revealed active myocarditis, with infiltration of the muscle by lymphocytes, neutrophils, macrophages and eosinophils, with considerable myocardial cell necrosis.
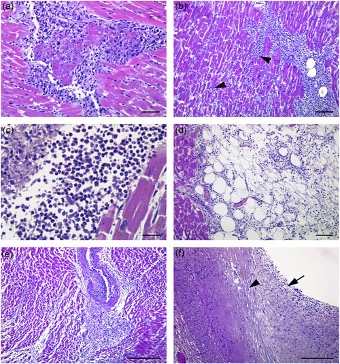
Figure 1 - “Pathological findings in the heart. (a–c) Active myocarditis characterized by lymphocytes, macrophages, neutrophils and eosinophils granulocytes associated with myocyte necrosis and myofiber disarray (arrowheads). (d) Pericarditis with lymphocytic inifiltration. (e) Necrotizing vasculitis with an inflammatory infiltrate formed by lymphocytes, monocytes, and eosinophils granulocytes. (f) Coronary artery with an inflammatory infiltrate of the tunica intima (arrow) and tunica media (arrowhead). H&E, haematoxylin and eosin. Scale bars: a = 28 µm; b, d = 56 µm; c = 14 µm; e, f = 200 µm” – Columbo et al.
PCR testing was performed in the heart muscle for nucleic acids from SARS-CoV-2, CMV, EBV, enterovirus, and HHV-6: only the PCR for HHV-6 was positive, and it was strongly positive. Thus, the heart pathology likely was caused by HHV-6, although co-infection by another infectious agent that encouraged reactivation of latent HHV-6 in myocardial tissue could have played a role.
This report did not distinguish HHV-6A from HHV-6B. The investigators also did not report whether they tested diseased lung, liver and skeletal muscle for various viruses, thus making it unclear if HHV-6 might have also been responsible for the co-existing pneumonia, hepatitis, skeletal muscle vasculitis or coronary artery endothelial inflammation. HHV-6 is known to cause pneumonitis with ground glass opacity (Sauter 2009), and can cause of fulminant liver disease (Raposo 2019, Phan 2017).
It remains possible that the primary cause of the heart, lung and liver pathology in this patient was SARS-CoV-2, despite the two PCR tests negative for SARS-CoV-2; latent HHV-6 in the diseased tissue could have been trans-activated by SARS-CoV-2. However, it seems at least as likely that the primary cause of the multi-organ pathology was reactivation of HHV-6.
Read the full article: Colombo 2022

