A recent review summarizes evidence that HHV-6 can cause endothelial dysfunction, which often is seen in both Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome.
Reactivation of latent herpesvirus infection—particularly EBV, HHV-6 and possibly HHV-7 —has been reported frequently in both Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Endothelial dysfunction also is seen in both illnesses.
Investigators from South Africa and the U.K. have published a review of the evidence that herpesviruses—particularly HHV-6, EBV and CMV—can infect the monolayer of endothelial cells that line blood vessels. A summary of the evidence regarding HHV-6 includes the following:
- HHV-6 is associated with greater endothelial damage than CMV (Caruso 2009, Takatsuka 2003)
- HHV-6 infects but does not kill endothelial cells (ECs), suggesting that ECs act as a reservoir for HHV-6 (Caruso 2002).
- HHV-6 maintains a low level of replication within the ECs (Rotola 2000, Shioda 2018).
- An association between HHV-6 and EC associated microcirculatory defects has been demonstrated (Vallbracht 2005).
- HHV-6 has been found in ECs of vascular tissue from patients with cardiovascular disease (Comar 2009, Leveque 2011).
- Cardiac dysfunction is associated with HHV-6 DNA persistence in endomyocardial biopsies (Escher 2015).
- HHV-6 infects the CNS and ECs lining the vasculature of the CNS (Harberts 2011)
- HHV-6 is considered to be a cause of myocarditis (Mahrholdt 2006).
- HHV-6, like EBV, uses TLR9 to upregulate inflammation and promote lymphocyte infiltration (Reynaud 2014).
- HHV-6 induces cellular inflammation and upregulates IL-8, RANTES and MCP-1 in ECs even during latency (Caruso 2002).
- Lymphatic vessel ECs are also susceptible to latent infection of HHV-6 (Caruso 2009).
The main points made by the review include the following:
- Herpesvirus infection of endothelial cells can cause endothelial dysfunction.
- Endothelial dysfunction can lead to vascular spasm and to increased coagulation, both of which can lead to diminished tissue perfusion which is common in Long COVID and ME/CFS patients.
- The fact that herpesviruses can chronically infect endothelial cells (which are long-lived) adds to the plausibility that chronic endothelial infection may be a factor in Long COVID and ME/CFS.
- The fact that reactivated latent infection can lead to infection of new endothelial cells is consistent with the waxing and waning pattern of symptoms seen in these two illnesses.
These ideas are graphically represented in the figure, below.
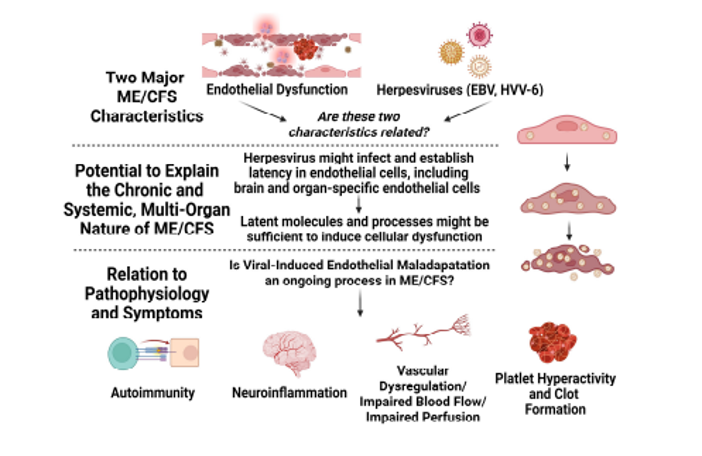
This review will be of interest to those interested in the evidence that HHV-6, CMV and EBV may be able to produce chronic endothelial dysfunction. Chronic endothelial dysfunction is unlikely to be the sole or primary cause of symptoms in Long COVID and ME/CFS. Many underlying abnormalities have been identified in both Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome. These include abnormalities of the immune system, central and autonomic nervous system, energy metabolism, the gut microbiome, and the cardiovascular system.
Read the full article: Nunes 2024