Although latent HHV-6 and HHV-7 were both more prevalent in the whole blood of fibromyalgia patients than in controls, only HHV-6 was found to be significantly correlated with nerve fiber damage severity. 51% of fibromyalgia patients had detectable HHV-6 DNA in whole blood compared to just 6% of controls. 17% of fibromyalgia patients had detectable DNA in the plasma compared to none of the controls.

Angelika Krumina, Santa Rasa, Simons Svirskis and Modra Murovska in the Murovska Lab at Riga Stradins University.
While HHV-6 has been a virus of interest in the context of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME), HHV-6 has not been studied in fibromyalgia, a related disease in several respects. Studies have found that up to 70% of people with fibromyalgia meet criteria for ME/CFS. Viral infections have been considered as possible triggers of both disorders, but so far, their exact roles have proved elusive. In the first study to examine potential HHV-6 involvement in fibromyalgia, a significant association was found between active or latent HHV-6 and nerve fiber damage among patients with the disease.
The investigators used quantitative sensory testing (QST) to determine the extent to which A delta and C nerve fibers were damaged. The unmyelinated C fibers are responsible for warmth sensation and deep and burning pain, while the thinly myelinated A delta fibers are involved in sensing cold sensation and sharp pain. Reduced or elevated sensation and/or pain to heat and/or cold in hands and/or feet represented abnormal QST findings. Of 43 patients, 39 (91%) showed abnormalities in 1-3 thermal QST modalities, which is indicative of light to severe A delta and C nerve fiber damage.
The team also performed qualitative, nested PCR on whole blood samples from patients and controls to test for presence of HHV-6 and HHV-7 DNA. They found that half of controls and 84% of patients had one or both viruses in their blood (p=0.013), and a significantly higher rate of HHV-6/7 coinfection was found among patients compared to controls (33% vs 5%, respectively). In total, HHV-6 genomic sequences were found in 23/43 (51%) patients vs 3/50 (6%) controls (p<0.001). There was less of a difference between prevalence of HHV-7 DNA among patients and controls, but like HHV-6, rates of detection were significantly higher among patients than controls (75.5% vs 52%).
Plasma viremia, which is considered a proxy for active infection, was only present in fibromyalgia patients (6/36, 17%); no active infection was detected in controls. Of the active infections, HHV-6 was found alone in 2 samples, HHV-7 single infection was found in 2 samples, and coinfections, in which both HHV-6 and -7 DNA were present in plasma, were also detected in 2 patients. Quantitative PCR determined that median HHV-6 and HHV-7 loads were higher in whole blood from patients compared to controls (815.8 and 311 copies/106 cells vs 125.5 and 173.12 copies/106 cells).
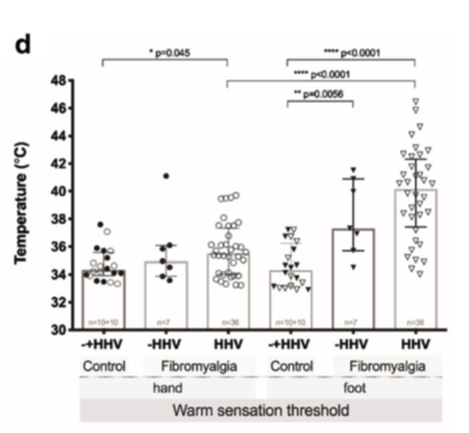 Among patients with active or latent HHV-6, abnormal QST results were more pronounced than in those without the virus in their whole blood or plasma. It remains to be determined whether the presence of HHV-6 and higher viral loads are a cause or effect of fibromyalgia, but it is known that HHV-6 infects nervous tissue and induces cellular dysfunction in affected areas. It is possible that persistent HHV-6 infection could directly or indirectly damage C and A delta nerve fibers, leading to fibromyalgia development and/or exacerbation.
Among patients with active or latent HHV-6, abnormal QST results were more pronounced than in those without the virus in their whole blood or plasma. It remains to be determined whether the presence of HHV-6 and higher viral loads are a cause or effect of fibromyalgia, but it is known that HHV-6 infects nervous tissue and induces cellular dysfunction in affected areas. It is possible that persistent HHV-6 infection could directly or indirectly damage C and A delta nerve fibers, leading to fibromyalgia development and/or exacerbation.
For more information on HHV-6 in diseases affecting the peripheral or central nervous system, visit our webpage on the topic.
Find the full paper here: Krumina 2019.

