Study does not address whether reactivated herpesviruses might be playing a role in the increased neurologic sequelae.
Past studies have suggested that several different infectious agents, including HHV-6, might be a trigger in the pathogenesis of Alzheimer’s disease (AD) and other dementias, although a role for HHV-6 remains controversial (Komaroff 2020). Moreover, some investigators doubt that any infectious agent is likely to be involved in the pathogenesis of AD.
A recently-published study from the US Department of Veterans Affairs compared over 135,000 people with SARS-CoV-2 infection (even mild COVID-19) to over 5 million people of similar age and sex who did not seek care for possible COVID-19, and followed them for three years. After using multivariate statistics to adjust for factors known to impact the risk of dementia, the investigators found that people with SARS-CoV-2 infection were nearly twice as likely to develop AD (HR 1.76-1.86 in years 2 and 3 following acute COVID-19).
The risk of multiple different neurological conditions including Bell’s palsy, dysautonomia, ischemic stroke, memory problems, loss of smell and taste, and peripheral neuropathy, was also significantly elevated in each of the first three years after acute COVID-19. It diminished somewhat in Years 2 and 3, but was still elevated. This progressively increasing risk was most evident among people hospitalized for COVID-19, but also was true for those with milder acute COVID-19, not requiring hospitalization, as shown in Figure 1.
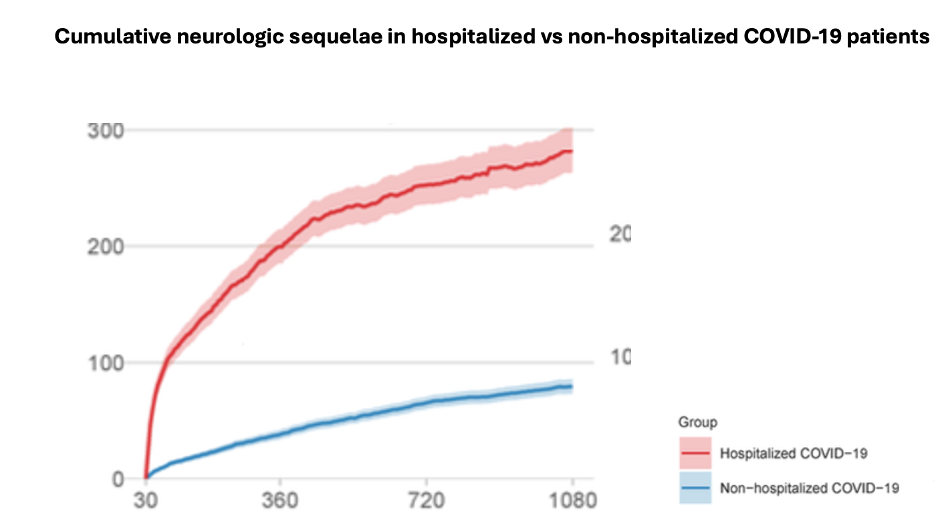
Cumulative number of post-acute neurologic sequelae by day. The center lines represent the adjusted cumulative excess number of events per 1000 persons in hospitalized (n=20,297) vs. non hospitalized (n=114,864) COVID-19 patients, compared to controls (n=5,206,835).
It appears that SARS-CoV-2 can infect the brain acutely, but evidence of persisting brain infection is mixed. It is possible that persisting residual reservoirs outside of the brain could elicit systemic inflammation that then triggers neuroinflammation (through both humoral and neural signals from the periphery to the brain).
Another possibility is that neurotropic herpesviruses reactivate during the COVID-19 illness, contributing to neurological impairment. Indeed, it has been shown in a number of studies that herpesvirus reactivation is common in severe COVID-19. A recent meta-analysis of herpesvirus reactivation in COVID-19 patients found the prevalence of active infection was 41% for EBV, 34% for HHV-6, 28% for HSV, 25% for CMV and 18% for VZV (Banko 2023).
Another study of severely ill COVID-19 patients found that 82% had reactivated EBV and 22% had clinically significant levels of HHV-6 DNA detected in whole blood (Simonnet 2021). Furthermore in a study of ICU patients in Brazil, 40% of patients with HHV-6 DNA detected in nasal swabs had CNS symptoms, compared to 14% of HHV-6 negative patients: the HHV-6 positive patients were also found to have increased expression of HHV-6 specific microRNA’s (Carneiro 2023).
Two limitations of the huge Veterans Affairs study must be acknowledged. First, studies of the clinical diagnoses recorded in the medical record—without a rigorous determination of the degree of possible over-diagnosis or under-diagnosis—should always be taken with a grain of salt. However, the huge size and resulting statistical power of this study is impressive. Second, based on population-wide studies by CDC, many of the 5 million people identified as not having been infected by SARS-CoV-2 must, in fact, have been infected but only mildly symptomatic or even asymptomatic.
Read the full article: (Cai 2024)

