Italian investigators found that 87% of patients with HHV-6 reactivations went on to develop a CMV infection, which occurred an average of 15 days later. On the other hand, in patients who did not reactivate with HHV-6, only 33% developed an active CMV infection.
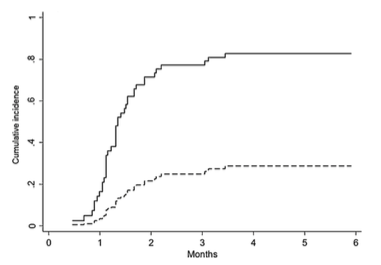
Cumulative incidence of CMV reactivation in patients with and without prior HHV-6 reactivation. Source: Journal of Clinical Virology, Crocchiolo 2016
The study was conducted retrospectively on 75 adult stem cell transplant patients who received T-cell replete grafts from HLA-haploidentical donors utilizing a high level of immunosuppression. Patients were tested twice weekly for the first 100 days. No CMV prophylaxis was administered.
Previous studies have also found a strong association between HHV-6 and CMV reactivation, and this may relate to the immunosuppressive effect of HHV-6 on T –cell functions. (Flamand 1995, Dagna 2012). HHV-6 can infect CD4+ lymphocytes and HHV-6A can also infect and replicate in CD8+ T cells and natural killer cells, and non-productive infection of macrophages and dendritic cells can result in dramatic functional abnormalities (Lusso 2006).
In a recent Japanese study on the impact of HHV-6 reactivation on outcomes in allogenic stem cell transplant patients, investigators reported that HHV-6 was associated with the development of acute GVHD and CMV reactivation, but that this phenomenon was most prominent in the setting of stronger immune suppression or myeloablative conditioning (Aoki 2015).
The authors note that HHV-6 is an indicator of cellular immunosuppression preceding CMV infection and suggest that further studies addressing the mechanism of the association are warranted.
For more information, read the full paper: Crocchiolo 2016.

