MS patients with a particular haplotype on natural killer cells are more susceptible to HHV-6A infection. Similarly, HHV-6A/B may contribute to Alzheimer’s by utilizing a specific NK cell inhibitory receptor to disrupt the ability of NK cells to clear infected cells.
An association between HHV-6, particularly HHV-6A, and Alzheimer’s disease (AD) has recently become a research topic of great interest, and efforts to explore the mechanisms behind this phenomenon are underway. Herpesviruses including HHV-6A/B have been found to induce beta-amyloid production (Eimer 2018) and HHV-6A and HHV-7 DNA and RNA is more prevalent and abundant in AD brains vs controls (Readhead 2018). NK cell dysfunction has been noted among AD patients, which is consistent with viral etiology.
 After isolating genomic DNA from the whole blood of 98 AD patients, the genotype of NK killer Ig-like receptors (KIR) was examined. The activating receptor KIR2DS2 and the inhibitory receptor KIR2DL2 were more frequently found in AD patients than controls, and they were found at similar frequencies (62% of AD patients vs. 37.2% of controls, and 62.2% of AD patients vs. 36.4% of controls, respectively). These two receptors are likely preferentially associated with each other, and when they are co-expressed, the inhibitory effects of KIR2DL2 override the activation of NK cells triggered by KIR2DS2. AD patients also had a lower frequency of KIR3DS1, an activating receptor. Together, these results indicated that the NK cells in AD patients might be in general less active than those in healthy individuals.
After isolating genomic DNA from the whole blood of 98 AD patients, the genotype of NK killer Ig-like receptors (KIR) was examined. The activating receptor KIR2DS2 and the inhibitory receptor KIR2DL2 were more frequently found in AD patients than controls, and they were found at similar frequencies (62% of AD patients vs. 37.2% of controls, and 62.2% of AD patients vs. 36.4% of controls, respectively). These two receptors are likely preferentially associated with each other, and when they are co-expressed, the inhibitory effects of KIR2DL2 override the activation of NK cells triggered by KIR2DS2. AD patients also had a lower frequency of KIR3DS1, an activating receptor. Together, these results indicated that the NK cells in AD patients might be in general less active than those in healthy individuals.
Additionally, a higher incidence of the HLA-C1/C2 genotype was seen among those with AD compared to controls. The combination of KIR2DS2, KIR2DL2, and the KIR ligand HLA-C1 was observed significantly more often among AD patients, and the presence of HLA-C1 in the absence of KIR2DS2 and KIR2DL2 was markedly lower than in controls. Notably, 14/20 patients who exhibited worsening of clinical manifestations at one -year follow-up possessed this combination of NK receptors and HLA genotype, and the combination was also associated with significantly lower Mini-Mental State Examination scores at diagnosis of AD. Moreover, the e4 allele of apolipoprotein E, which is the least effectual allele in clearing beta-amyloid and increases the risk for AD, was also associated with the KIR2DS2/KIR2DL2/C1 combination, and it was more frequent among AD patients on the whole (40.4%) compared to controls (14%). HHV-6A was found to increase apolipoprotein E e4 mRNA synthesis.
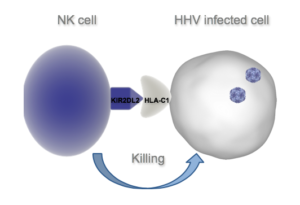
The group also evaluated HHV-6A infection in the presence of KIR2DL2 expressing cells to determine whether the KIR2DS2/KIR2DL2/C1 combination might increase a person’s susceptibility to HHV-6 infections. While wild-type NK cells were able to effectively kill HHV-6A-infected T cells expressing the HLA-C1 allele, NK cells with KIR2DL2 expression were not able to do so. Furthermore, HHV-6A induced PKA activity and phosphorylation of Sp1 in the NK cells, which may increase expression of KIR2DL2 and thereby inhibit NK cell cytotoxicity. The authors also noted that the HHV-6A-induced expression of apolipoprotein E e4 may further inhibit NK cell function, in part by increasing PKA activity.
The diminished ability of KIR2DS2/KIR2DL2 expressing NK cells to clear HHV-6-infected cells with HLA-C1 present, paired with the increased frequency of this KIR/HLA combination among AD patients, suggests that underlying genetic factors may predispose to ineffective clearance of HHV-6(A). Consequently, HHV-6 infections may persist in the central nervous system and contribute to AD development and worsening. If this is confirmed, modulation of KIR2DL2 expression could represent a novel therapeutic target for AD, and anti-herpesvirus medications may be options to consider in those suffering from AD.
Interestingly, KIR2DS2/HLA-C1 and KIR2DL2/HLA-C1 combinations have been found to be less frequent among patients with acute viral encephalitis compared to healthy controls (Tuttolomondo 2018).
The use of whole blood to determine KIR/HLA haplotype makes this a relatively non-invasive procedure that could enable its use as a broad-scale screening tool for AD risk factors.
Find the full paper here: Rizzo 2019.

