It is unknown whether high viral loads correlate with worse prognosis.
Detection of HHV-7 in the lungs has been identified as a risk factor for interstitial pneumonia or idiopathic pulmonary fibrosis (Yamamoto 2005; Sheng 2020)
HHV-7 DNA is occasionally reported in the bronchioalveolar lavage (lung) specimens of people with severe pneumonia, particularly when they are immunocompromised. However, the studies have been small, and have not provided evidence that HHV-7 is a cause of pneumonia or that, when present, it increases the severity of pneumonia.
What may be the largest study of this question has recently been reported: a retrospective cohort study in adults with severe pneumonia requiring mechanical ventilation, from 12 centers in China. About 25% of the patients were immunocompromised. Bronchioalveolar lavage fluid was tested by metagenomic next-generation sequencing to identify viral DNA. Unfortunately, since mNGS testing is not quantitative, the investigators were not able to compare higher viral loads (likely to predict poor outcome) to those with low-level infection.
Out of a total number of 721 such patients, 45 (6.24%) had evidence of HHV-7 DNA in the lower respiratory tract. HHV-7 positive patients were more likely also to have other herpesviruses detected in the same lavage fluid than were HHV-7 negative patients: human cytomegalovirus (42.2% vs 20.7%, p = 0.001) and Epstein–Barr virus (35.6% vs 18.2%, p = 0.008).
The HHV-7 positive patients were compared to the HHV-7 negative patients, after using statistical techniques to take into account other factors that might have affected the severity and outcome of the pneumonia. There was no significant difference between the two groups in the total length of hospital stay (30.4 vs 30.7, p = 0.942).
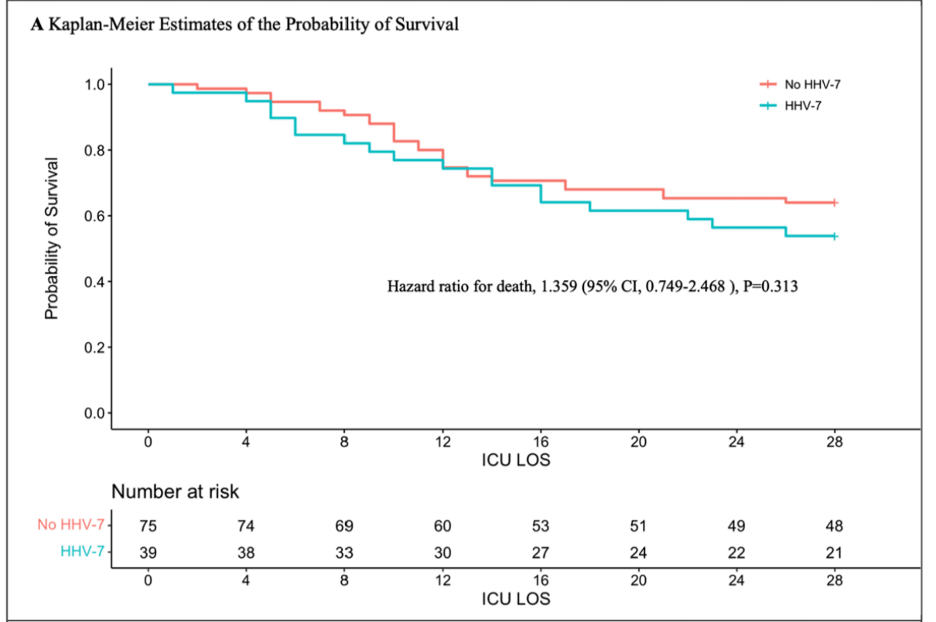
Multivariate analysis showed that HHV-7 positive was associated with a somewhat higher 28-day mortality (HR 1.783), although this finding was not statistically significant (p = 0.079). The slight superiority of the survival curve for the HHV-7 negative patients (Figure 1, below) also was not statistically significant. However, as the authors acknowledge, even though this may have been the largest study of this question, it still was small enough that the study had poor power to recognize these differences as significant.
The study found a suprisingly low level of HHV-6B (2% in the HHV-7 negative patients and 4.5% in the HHV-7 positive patients), which may be a reflection of the mNGS technique used, or a lower prevalence in China. A study at the University of Washington, using quantitative PCR on 557 lung samples, found HHV-6B in 27%. Furthermore, they demonstrated that HHV-6B infection doubled the mortality rate of transplant patients with respiratory infections (Hill 2019). HHV-6B reactivation also increases the risk of idiopathic pneumonia syndrome (Zhou 2019).
This Chinese study does not provide convincing evidence that HHV-7, when identified in bronchioalveolar lavage fluid from patients with severe pneumonia, is causing the pneumonia or worsening its severity. However, there are trends that suggest the presence of the virus may be linked to worse outcomes: these trends should be pursued by even larger studies.
Finally, it is interesting that HCMV and EBV were detected more frequently in HHV-7 positive patients. Did this simply reflect the fact that immunosuppression and chronic disease encouraged the reactivation of these latent viruses? Or might reactivation of one of these three herpesvirus have transactivated the others?
Read the full article: Xu 2023

