The inflammation seen during acute COVID-19 can trigger reactivation of latent herpesviruses. This, in turn, could theoretically contribute to the hyperinflammatory state and generation of autoantibodies sometimes seen in acute COVID-19. How often are EBV and HHV-6 reactivated during acute COVID-19?
Investigators at the University of Virginia evaluated 67 patients hospitalized for acute COVID-19 who had high levels of at least one of two inflammatory markers: C-reactive peptide (CRP) and D-dimer. They used a quantitative real-time PCR assay capable of detecting 50 copies of viral DNA per ml of plasma, and looked for viral DNA in blood on one occasion at about day 7 of hospitalization.
The team found that 22.4% (15/67) of acute COVID-19 patients had detectable EBV DNA and 4.5% (3/67) had detectable HHV-6 DNA in the plasma. This level of plasma viremia is significantly higher than has been reported in plasma testing of healthy cohorts. The authors noted that there are large differences in various assays of reactivation, making comparisons with previous studies difficult.
One issue with this study is that involved plasma, and EBV DNA and HHV-6 DNA can be found in whole blood and PBMCs at far higher rates and levels than in plasma. HHV-6 DNA is found in 1% or less in healthy controls (Chapenko 2003, Berti 2002) and EBV is typically found in fewer than 10% plasma in healthy controls (Chan 2018, Lin 2004). Unfortunately, the authors compared their plasma DNA results to control studies that used cellular samples for testing, understating the significance of their findings.
The investigators also looked at whether markers of inflammation were correlated with evidence of reactivation, and found no statistically significant correlation, although the number of people with reactivated HHV-6 was small: therefore, the study was poorly powered to identify a significant correlation (Figure 1).
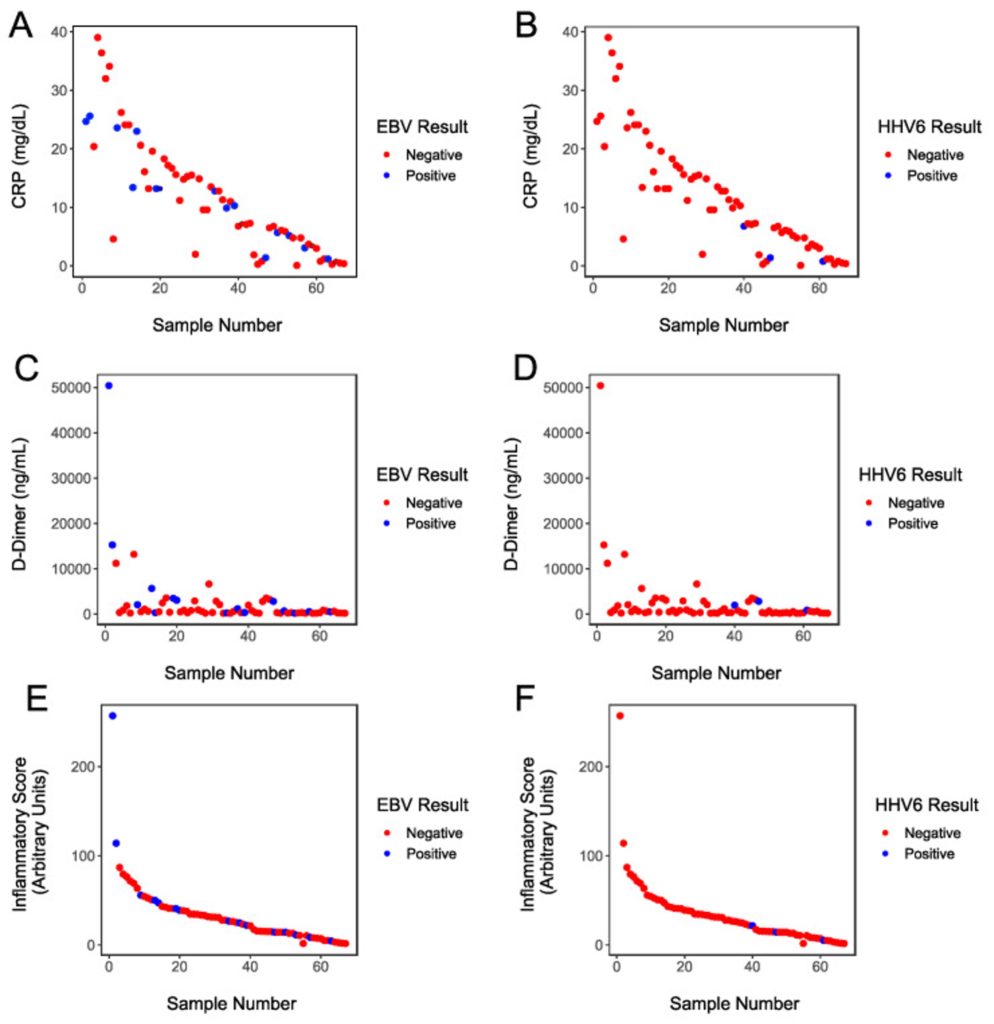
Figure 1 – CRP level, D-dimer level, and composite inflammatory score plotted against “positivity” (viral load above 50 copies/ml plasma), with blue indicting EBV positive patients and red indicating HHV-6 positive patients. No statistically significant correlations were identified.
This study evaluated an important and plausible hypothesis, using appropriate technology, and did not find strong evidence in support of the hypothesis.
However, the study authors recognize several limitations:
- The study examined only patients for whom CRP and D-dimer had been obtained during hospitalization, and such people may not have been representative of all patients hospitalized for acute COVID-19;
- No healthy control group without COVID-19 was evaluated using the same assay;
- By assessing viral reactivation at only one point in time, at around 7 days of hospitalization, the study was not able to evaluate the possibility of delayed reactivation, as has been demonstrated for HHV-6 viremia in people with Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) syndrome as well as in hematopoietic cell transplant patients (approximately 20 days post-transplant).
The study also was not designed to test the possible role of reactivation of these viruses in those individuals who go on to develop post-acute-COVID-19 syndrome, or “Long COVID”. Other studies have found that reactivation of EBV may occur more commonly in people with Long COVID than in post-COVID-19 patients who do not develop Long COVID (Su 2022).
Finally, plasma may be the wrong compartment to determine the true impact of herpesvirus reactivation. Elevated levels of HHV-6, CMV and EBV have been found in the bronchioalveolar lavage (BAL) and lung tissue of patients with “idiopathic” pneumonia in the absence of significant plasma viremia.
A 2021 study of nasopharyngeal samples of 60 SARS-CoV2 patients admitted to the hospital found that 23% of the COVID+ samples were also positive for HHV-6 DNA, and that HHV-6 was more prevalent in younger patients and those taking immunosuppressants (Lino 2021).
Another study of HHV-6 DNA in nasal swabs in patients with severe COVID-19 found that 40% of the patients with HHV-6 DNA had CNS symptoms compared to 14.3% of those who were negative (de Souza Carneiro 2022).
Thus, the evidence that reactivation of HHV-6A/B and HHV-7, and other herpesviruses, may contribute to the inflammatory state in people with COVID-19 remains mixed.
Read the full paper: Brooks 2022