Previous research has found a correlation between HHV-6A infection and primary unexplained infertility, preeclampsia and congenital infection, and the mechanisms involved suggest it might play a role in intrauterine growth restriction (IUGR) as well (Komaroff 2021). Indeed, viral infections within the first 6-8 weeks have been linked to intrauterine growth restriction (IUGR) (Waldorf 2013), and several human herpesviruses—CMV, HSV-1, VZV, and HHV-8—have been associated with IUGR, but HHV-6 has not previously been studied.
Researchers from the Sant’Anna Hospital in Ferrera hypothesized that HHV-6 might be one viral trigger of IUGR. 11 women with late-onset IUGR and 11 control women with normal, physiological pregnancies were included, and their placentas were examined histochemically to semiquantitatively assess levels of HHV-6 antigens (making no distinction between HHV-6A and -6B).
The IUGR group had a significantly higher percentage of placental tissue with positive HHV-6 than did the healthy control group (81.9% vs 9%, p = 0.0001). Of the HHV-6-positive HHV-6 IUGR cases, 40% of invasive extravillous trophoblast (EVT) had HHV-6 staining as compared to 0% in the HHV-6 positive healthy control group (p=0.0001). Of the positive HHV-6 IUGR, 63% of the syncytiotrophoblasts had HHV-6 staining as compared to 9% from the HHV-6 positive control samples (p=0.0001).
Interestingly, the IUGR cases showed a higher density of HLA-G than the control cases (p<0.0001). HLA-G, a nonclassical class I major histocompatibility complex is an immunosuppressive molecule that reduces an attack on paternal antigens by NK cells and T cells. However, particularly when it is expressed by endothelial cells, it also inhibits angiogenesis—an important component of uterine implantation. In the IUGR group, HHV-6 positivity correlated with higher HLA-G as well (p < 0.05). Previous research has found that the HHV-6 U94 protein can up-regulate the expression of HLA-G in placenta, which impairs the angiogenesis important in implantation (Rizzo 2018).
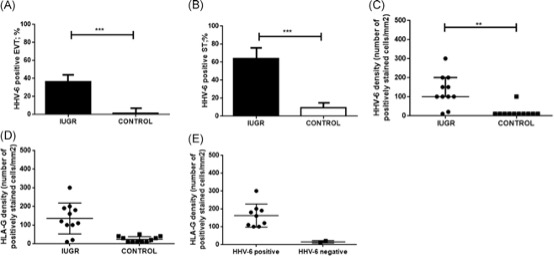
Percentage of HHV-6 positive samples in invasive EVT cells (a) and syncytiotrophoblast cells (b), number of HHV-6 positive cells/mm^2 (c) , and number of HLA-G positive cells/mm^2 (d) between IUGR/control placentas. Also, number of HLA-g positive cells/mm^2 between HHV-6 positive and negative cells for both IUGR/control placentas (e).
While the sample size of this study is small, it demonstrates a strong association between HHV-6 infection of the placenta and intrauterine growth restriction, and suggests plausible mechanisms by which HHV-6 might impair implantation and lead to growth restriction. This finding parallels previous reports linking HHV-6 infection of endometrium and higher density of HLA-G with primary idiopathic infertility (Marci 2016, Caselli 2017), another condition in which defective implantation is involved. Indeed, it seems plausible to consider IUGR a milder consequence of defective implantation than primary infertility: fetal growth is restricted, but fetal life is not ended.
Read the full article: Bortolotti 2021

