Cytokines IL-4, IL-8 and IL-10 correlated with graft rejection and were elevated in HHV-6+ patients.
Among the human herpesviruses that may influence the success of engraftment in organ transplantation, Epstein–Barr Virus (EBV) and cytomegalovirus (HCMV) have been studied the most. A team from several institutions in Mexico City studied pediatric solid organ transplant (SOT) recipients who had undergone either liver or kidney transplantation. From 20 such patients,158 serial blood samples were obtained.
The following measurements were made from the blood samples:
- Levels of 17 cytokines using a Bio-Plex assay: IL-1β, IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, IL-12, IL-13, IL-17A, IFN-γ, TNFα, MCP-1, MIP1-β (macrophage inflammatory protein 1β), G-CSF (granulocyte-colony stimulating factor) and GM-CSF;
- Herpesvirus DNA, using an in-house multiplex qPCR that simultaneously detects and quantifies beta and gamma human herpesviruses, and that could not differentiate HHV-6A from HHV-6B.
The following observations were made:
- Elevation of IL-4, IL-8, and IL-10 correlated with graft rejection (see Figure 1, below);
- Different human herpesviruses were associated with different patterns of cytokine expression (see Figure 2, below);
- Three cytokines were elevated in samples where HCMV or HHV6 were detected alone or where EBV and HHV7 were co-detected;
- Single HHV-6 DNAemia was associated with increased TNFa, IL-4, MCP-1 and IL-10
- Multiple viral DNAemia that included HHV-6 was associated with increased IL-12, IL-2, IL-10, IL-4
- When EBV DNA was detected without reactivation of other herpesviruses there appeared to be an immunomodulatory effect: multiple cytokine levels were reduced;
- However, when HHV-6 or HCMV were detected along with EBV, there were heightened cytokine levels in the blood, and graft rejection.
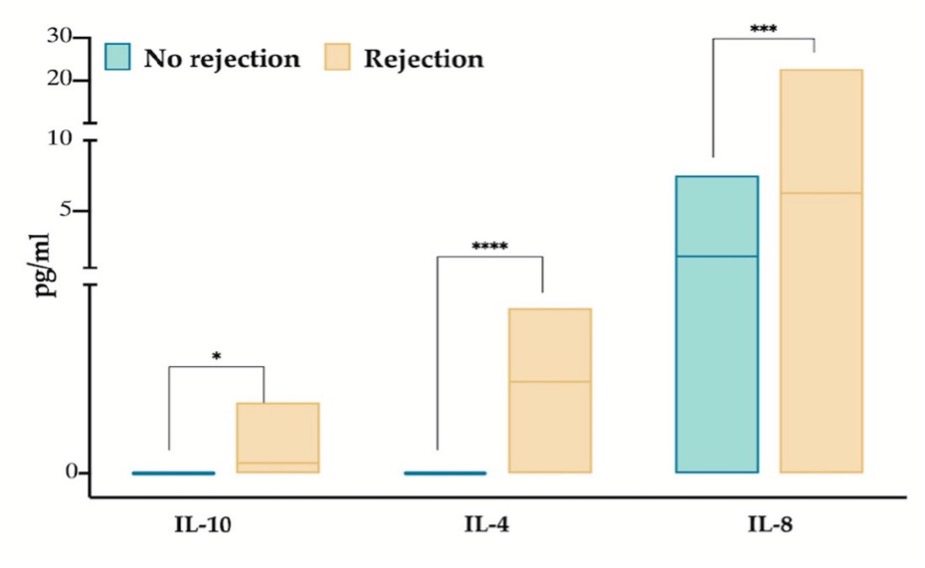
Figure 1. Levels of three cytokines were significantly greater in patients undergoing graft rejection.
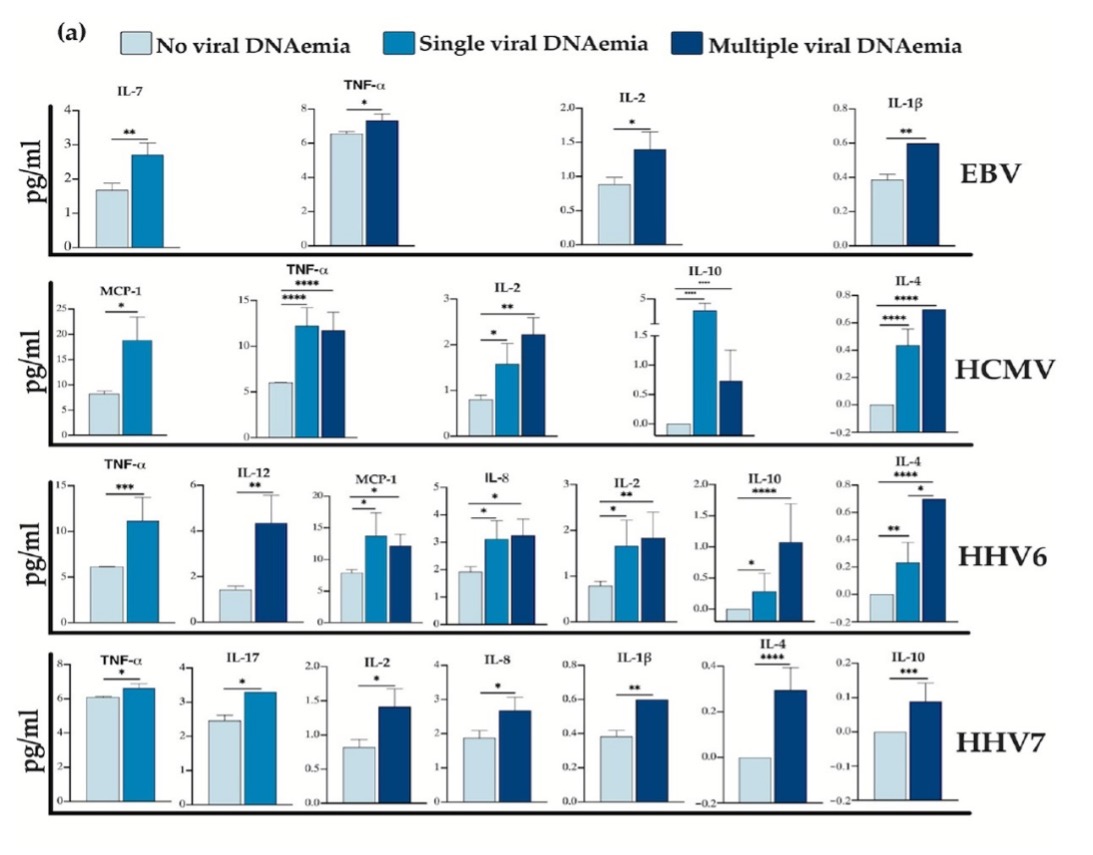
Figure 2. Levels of different cytokines in patients with no viral DNA detected, patients with DNA from a single virus detected, or DNA from multiple viruses detected.
A previous study at University of Pittsburgh showed that high level HHV-6 viremia is associated with allograft rejection at 100 days (Singh 2021) and a study at Baylor showed that seronegative pediatric liver transplant patients frequently acquire clinically significant HHV-6 infections from the organ donor (Mysore 2021).
The current study presents a series of correlations that suggest, but do not prove, that HHV-6 reactivation may influence the course of solid organ transplantation in pediatric patients.
Read the full text: Sánchez-Ponce 2024