CD8+ T cells recover but CD4+ T cells remain low
Investigators in France discovered that monocytes and B lymphocytes recover quickly and become abnormally elevated by day 75 in double cord blood transplant patients (dUCB), while they remained below normal or normal in allogeneic stem cell transplant (allo-HSCT) patients who received unrelated peripheral blood stem cells (uPBSC). CD4+ T cells remained significantly below normal levels for six months in both groups.
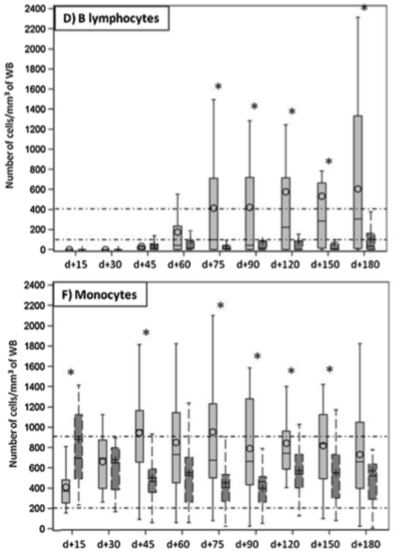
While CD4+ and CD8+ T cells remained at below normal levels throughout the first six months, monocytes in the dUCB group (light grey) jumped to higher than average levels by day 45, and B lymphocytes were elevated compared to the group receiving uPBSC (dark grey) by day 75. Source: Journal of Clinical Virology
HHV-6 and BK virus DNA levels were significantly higher in cord blood transplant patients, while EBV DNA load was significantly higher in the allo-HSCT group. CMV viral load was the same in both groups.
HHV-6 active infection was found in 84% of dUCB compared to 21% of uPBSC patients. HHV-6 infections occurred within the first month and were persistent over the first year, lasting up to four years in half of the dUCB patients.
Some investigators have hypothesized that CD134 expression differs by graft type and that this may explain the higher rate of HHV-6B reactivation in cord blood transplants, but warn that a yet unknown factor in the cord blood graft or during immune reconstitution may increase the risk of HHV-6B infections.
This study confirmed that HHV-6 infection results in delayed engraftment and a higher need for blood and platelet transfusions. Of interest, neither HHV-6 encephalitis nor increased transplant related mortality was seen in the dUCB cases, in contrast to previous reports. They attribute their success to the use of a reduced intensity conditioning regimen and the fact that they only rarely use anti-thymocyte globulin (ATG) for their cord blood patients.
ATG, a risk factor for HHV-6 encephalitis, was used in the uPBSC group, and the authors speculate that this may be the reason behind the increased EBV reactivation in uPBSC patients compared to the dUCB group.
The authors noted that CD4+ T cell levels rose faster after dUCB transplantation while CD8+ T cell levels rose faster after uPBSC. A majority of the patients (66%) had several viral infections, suggesting to the authors that trials for therapeutics that work on multiple infections might be useful.
Read the full paper: Illiaquer 2017.

