Josh Pritchett, University of Minnesota Medical School
A group from the University of Minnesota studied the T cells of umbilical cord blood transplant patients and found that CD4+ T lymphocytes co-expressing CD134 contained more than twice the level of HHV-6B than cells without CD134 expression. This study adds clinical confirmation to the recent discovery that CD134 is a cellular entry receptor for HHV-6B. In addition, this study also suggests that there may be other means of viral entry yet to be discovered, as the group found a majority of patients (nearly 70%) had CD134 negative cells infected with HHV-6B.
The investigators used a highly sensitive assay to measure the viral load in CD134+ and CD134- T cells in blood samples from 20 patients taken 28 days post-transplant. After ciHHV-6 or HHV-6A+ patients were excluded, the remaining 16 patients had HHV-6B at a mean concentration of 0.308 copies in CD4+ CD134+ cells versus 0.129 copies in CD4+ cells that were CD134 negative (p=0.0002).
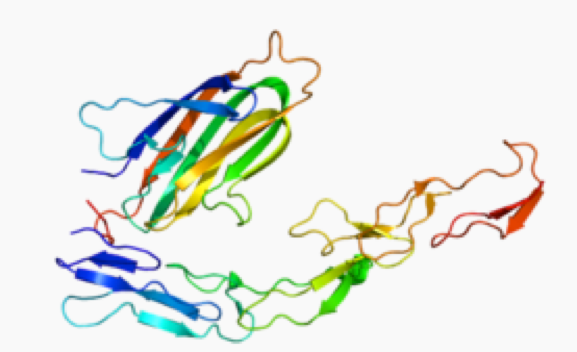
CD134, a member of the tumor necrosis factor receptor superfamily (TNFRSF4) also known as OX40, was recently identified as a receptor for HHV-6B (Tang 2013), and is only expressed on T cells after they have been activated. Although HHV-6B was more common in CD134+ cells by a factor of five-fold in the present study, one patient was found to have more HHV-6B in the CD134- cells.
“Although our data certainly suggest that CD134 expression is an important contributing factor to HHV-6B infection or dissemination after transplant, they also seem to indicate that there are other elements at play which have yet to be discovered.” said Pritchett, lead author of the study.
The authors note that the higher levels of HHV-6B in the CD134+ cells could have been a result of viral reactivation and recent infection of such cells after transplant. “The fact that HHV-6B DNA was also detected in CD134- cells suggest there is possibly another receptor, that levels of CD134 were below the detection limit, or that the cell stopped expressing it after a while,” commented immunologist Louis Flamand, PhD.
Of note, the expression of CD134 on CD4+ and CD8+ T cells has been previously associated with the development of acute and chronic graft versus host disease (aGVHD) (Blazar 2003) and selective depletion of CD134+ cells, and it has been explored as a means of reducing aGVHD without a loss of pathogen specific immunity (Ge 2008).
A recent study also found that CD134 is preferentially expressed in CD4+ cells of patients with drug induced hypersensitivity syndromes (DIHS) or drug reaction with eosinophilia and systemic symptoms (DRESS) (Miyagawa 2016).
This work represents an important step in characterizing the cellular mechanism of post-transplant HHV-6B reactivation, a poorly understood event that occurs in an estimated 50-70% of all umbilical cord blood transplant patients. Further studies comparing CD134 expression among recipients of different stem cell sources and confirmation of CD134 as an important factor in HHV-6 reactivation post-transplant may help to explain the increased rates of reactivation after UCBT and may also lead to the identification of novel targets for immunotherapy, and consequently, more effective treatment options for the prevention of adverse outcomes related to HHV-6B reactivation in immunosuppressed individuals.
The receptor for HHV-6A is CD46, and CD134 was identified as a receptor for HHV-6B in 2013. A CD46 transgenic mouse model was developed in France (Reynaud 2014). There is currently no mouse model for HHV-6B.
Read the full paper here: Pritchett 2016.