Dutch investigators found that hematopoietic cell transplant (HCT) patients with high levels of HHV-6 viremia have reduced late immune reconstitution while early reconstitution was not affected. On the other hand, patients treated with antiviral therapy had normal immune reconstitution. The authors conclude that intensive monitoring with more aggressive antiviral treatment could improve outcomes in patients with high HHV-6 viral loads.
The group, led by Jaap-Jan Boelens at University Medical Center Utrecht (UMC), reported that every increase of 10,000 HHV-6 copies/mL plasma correlated with an 8.7% decrease in CD4+ count. This effect was only observable after 250 days post-HCT (i.e. within the late thymus-dependent phase of CD4+ reconstitution), suggesting that HHV-6 viremia could be hampering thymopoiesis, or the process by which thymocytes differentiate into mature T lymphocytes.
T-cell reconstitution after HCT has two phases: 1) an immediate, thymus-independent phase, in which T-cell reconstitution takes place primarily in the periphery, and 2) a late, prolonged, multi-step, thymus-dependent phase that can take up to 18 months after HCT. The authors postulated that homeostatic peripheral expansion could be efficiently replacing CD4+ cells depleted by HHV-6 in the early phase, whereas the human body does not have sufficient mechanisms to overcome the effects of HHV-6 in the late thymus-dependent phase of immune reconstitution after HCT. This speculation is corroborated by the observation that HHV-6 affected only naïve CD4+ reconstitution after day +300 post-HCT and not effector memory CD4+ reconstitution in their 273 pediatric patients (p=0.028).
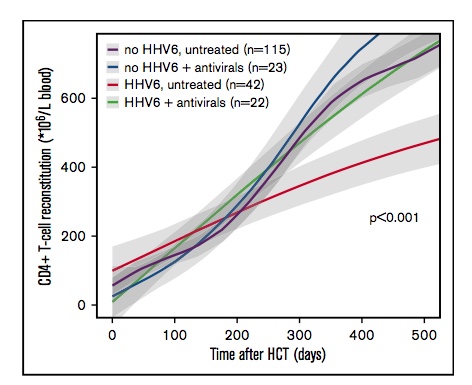
CD4+ T-cell reconstitution in un treated vs treated patients with HHV-6 viremia. Source: blood advances, ASH 2018.
CD4+ reconstitution was not delayed in patients with HHV-6 viremia who had received antivirals (cidofovir, ganciclovir, and foscarnet). These patients received the antivirals for a variety of indications not limited to symptomatic HHV-6 reactivation (e.g. CMV or AdV reactivation). They reported that antiviral treatment increased the chance of successful CD4+ reconstitution by 42.8%, despite viremia. This level of immune reconstitution was significantly better than that of patients who reactivated HHV-6 but were not treated with antivirals (p<0.001); furthermore, patients who reactivated HHV-6 but were treated with antivirals had CD4+ reconstitution comparable to that of patients without HHV-6 reactivation at all.
The authors note that the impact of HHV-6 viremia on immune reconstitution was dependent upon a high viral load; for every 105 HHV-6 copies/ml plasma, CD4+ reconstitution was at risk of dropping about 9%.
Timely CD4+ T-cell immune reconstitution after allogeneic hematopoietic stem cell transplantation is associated with increased survival and lower transplant-related mortality (Admiraal 2015, Admiraal 2016, Fedele 2012). Previously, many researchers have hypothesized that the delay or absence of CD4+ immune reconstitution creates an opportunity for endogenous reactivation of latent viruses, including HHV-6, which is known to infect and kill CD4+ cells (Takahashi 1989, Yasukawa 1998).
Last year, the same authors published a study of 273 pediatric alloHCT patients at UMC showing that patients who reactivated HHV-6 were more than 3 times likelier to develop grade 2-4 acute graft-versus-host disease (HR 3.47, p<0.0001). Furthermore, they demonstrated that delayed immune reconstitution made aGVHD even more likely in patients who reactivated HHV-6 (p=0.0074) (Admiraal 2017).
Having shown that HHV-6 viremia increases the risk of developing aGVHD, an effect ameliorated by successful T-cell reconstitution, these investigators sought to determine whether HHV-6 viremia impedes CD4+ reconstitution or vice versa (i.e. delayed CD4+ reconstitution leads to HHV-6 viremia).

Jaap-Jan Boelens of the Laboratory of Translational Immunology and the Pediatric Blood and Marrow Transplantation Program, UMC, The Netherlands.
Studies are needed to determine whether monitoring CD4+ T-cell recovery concomitantly with HHV-6B reactivation after alloHCT could identify patients at risk for development of aGVHD and delayed immune reconstitution, allowing for more targeted antiviral therapy, an approach that has proven to be effective for CMV reactivation (Krawczyk 2018).
Read the full study: de Koning 2018.

