Investigators at the University of Minnesota found that cord blood transplant cancer patients with HHV-6B reactivation in the first 28 days are almost 4x more likely to relapse in the first two years compared to those with no early reactivation.
The team studied HHV-6 reactivation by day +28 post-CBT as well as 2-year cumulative incidence of relapse in 152 patients receiving cord blood transplants for blood cancers. Only 32 (21%) did not reactivate HHV-6. These patients were significantly less likely to experience relapse in both univariate (26% vs. 7%, p=0.03) and multivariate analyses (HR 0.2 [0.05-0.9], p=0.03). The authors suggested that CB allografts have a powerful graft-versus-tumor (GvT) effect when the grafts are not complicated by HHV-6 reactivation.
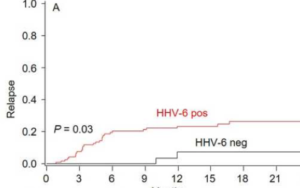
Relapse rate in those with early HHV-6 reactivation compared to those with no reactivation, in cord blood transplant patients with blood cancers. Source: American Journal of Hematology
Of the 152 total patients who were regularly surveilled for HHV-6 reactivation, 31 relapsed a median of 137 days post-CBT; 29 of these 31 patients reactivated HHV-6 by day +28. The investigators used a refined disease risk index to exclude the possibility that lower relapse rates among patients without HHV-6 reactivation were simply due to more favorable-risk diseases.
Past studies have associated HHV-6 reactivation after alloHCT with increased non-relapse mortality (Aoki 2015) and lower overall survival (Gotoh 2014). However there have been conflicting results as well (Cirrone 2016, Verhoeven 2015). These varied results are likely due to differences in institutional protocols and clinical practice regarding HHV-6. It is also possible that some centers administer more aggressive CMV prophylaxis/treatment than others, which could mask the effects of HHV-6 (Violago 2015). Although their data remain to be reproduced, the University of Minnesota study provides us with more insight into the role of HHV-6 in transplant patients. It is unclear whether HHV-6 was directly involved in the relapse process or if it is merely a sign of poor immune function. The team attempted to reconcile their findings by comparing NK cell counts of patients with HHV-6 reactivation to those of patients without HHV-6 at day +28, but found no difference between the two groups. Unfortunately, the investigators were not able to monitor NK cell function or NK cell counts in subsequent months.
Similarly, the group found no difference in the CD4+ cell counts in patients with and without HHV-6 reactivation by day +28, but did not measure long-term (after day +200) CD4+ reconstitution. A recent study from the University Medical Center Utrecht (UMC) found that early reconstitution was not affected by HHV-6 reactivation, but noted that patients with untreated HHV-6 reactivation had significantly lower CD4+ counts after day +200 (patients with HHV-6 reactivation who were treated with antivirals had normal CD4+ counts after day +200). Every increase of 10,000 HHV-6 copies/mL plasma led to an 8.7% reduction in CD4+ reconstitution in alloHCT patients (de Koning 2018).

Daniel Weidorf, MD, University of Minnesota
Given the association HHV-6 has with encephalitis (Scheurer 2012), aGVHD (Phan 2018), relapse, and reduced survival, further studies are needed on the effects of HHV-6 reactivation in transplant patients. Furthermore, clinicians need better therapies as current prophylaxis/therapies are not sufficiently efficacious and come with toxic side effects (Ogata 2013, Ogata 2018).
The University of Minnesota study was led by Daniel Weisdorf, MD.
Read the full paper here: (Rashidi 2018).

