A team at Stanford University led by Olivia Martinez, PhD, reported that HHV-6 was detected nearly twice as often in children transplanted for liver failure of unknown etiology (LFUE) compared to age-matched controls transplanted for metabolic liver disease (66.7% vs. 37.3%, p=0.005). In particular, HHV-6 was detected more often in LFUE patients less than 3 years old vs. control patients less than 3 years old (48.1% vs. 7.4%, p=0.0009).

Olivia Martinez, PhD, Professor of Surgery, Stanford Biosciences
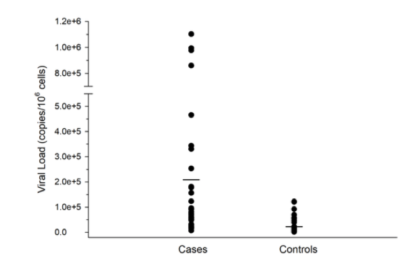
Furthermore, the HHV-6 viral load was significantly higher in LFUE cases compared to controls (mean 213,207 copies/106 cells vs. 38,115 copies/106 cells, p=0.0008). As a result, Stanford has now instituted routine evaluation for HHV-6 in all children who present with LFUE.
Formalin-fixed paraffin-embedded samples from 62 liver explants were studied, as well as 51 age-matched controls. Overall, the average age for both the 51 LFUE patients and 51 age-matched controls was 4 years. The quantitative PCR assay used had a lthreshold of 1.0x103 copies copies/mL and did not distinguish between HHV-6A and HHV-6B.
Among patients with detectable HHV-6, the mean tissue HHV-6 DNA load was 2.1x105 copies/106 cells in LFUE cases (range: 7.3x103 – 1.1x106) vs. 3.8x104 copies/106 cells in controls (range: 1.4x103 – 1.2x105) (p=0.0008). HHV-6 was detected more often in LFUE cases vs. controls in patients 6 years or younger (22/38 vs. 8/38, p=0.002), but not in children 6 years or older (12/13 vs. 11/13, p=0.61).
This finding was even more pronounced in children less than 3 years old, in which HHV-6 was detected nearly 7 times as often in LFUE cases compared to controls.
 Past studies have shown that the probability of liver graft survival was less than 60% at 500 days in patients with high HHV-6 levels in the liver graft (>11.27 copies/103 cells) and was only 40% at 500 days in those with HHV-6 found in the peripheral blood (compared to >80% in controls) (Pischke 2012). Several cases of LFUE associated with HHV-6 have been reported, particularly in younger children (Ostapowicz 2002, Ishikawa 2002, Asano 1990, Harma 2003, Harma 2013).
Past studies have shown that the probability of liver graft survival was less than 60% at 500 days in patients with high HHV-6 levels in the liver graft (>11.27 copies/103 cells) and was only 40% at 500 days in those with HHV-6 found in the peripheral blood (compared to >80% in controls) (Pischke 2012). Several cases of LFUE associated with HHV-6 have been reported, particularly in younger children (Ostapowicz 2002, Ishikawa 2002, Asano 1990, Harma 2003, Harma 2013).
Given that LFUE has a poorer short-term transplant-free survival compared to other causes of fulminant hepatic failure, this study represents a critical step in identifying possible etiologies of LFUE. Other viruses, including hepatitis A-C, EBV, and CMV, have been extensively studied as possible causes of LFUE, however these viruses are negative in LFUE (Chevret 2008, Yang 2018).
One limitation of this study is that the HHV-6 infection was not localized to a certain cell type. HHV-6 is a lymphotropic virus, although several studies have been able to localize HHV-6 DNA to hepatocytes by in situ hybridization (Ishikawa 2002, Ozaki 2001) and in vitro studies have shown that HHV-6 can infect the human hepatoma cell line HepG2 and cause hepatic cell injury (Cermelli 1996, Inagi 1996).
The authors called for further investigation of the role of HHV-6 in LFUE, with an emphasis on those younger than 3 years of age and plan to study whether antiviral therapy can improve the clinical course for these patients.
Read the paper: Yang 2018