Herpesvirus co-infections, particularly HHV-6 and CMV cause severe lymphopenia, pneumonia, and an increased risk of acquiring bacterial and fungal infections in non-transplant acute leukemia patients undergoing chemotherapy.
Severe lymphopenia (ALC <500/uL) occurred more often in those with co-infections compared to single infections (p<0.001). Those with co-infections also had significantly more occurrences of rash (p=0.04), pneumonia (p=0.008), bacteremia (p<0.001), and fungal co-infections (p=0.038).
In this prospective study of 95 patients French researchers obtained blood samples from newly diagnosed acute leukemia patients at the time of diagnosis (before chemotherapy), during chemotherapy, as well as post-induction, post-remission, and post-salvage chemotherapy and tested for herpesvirus (HSV-1/2, VZV, EBV, CMV, HHV-6A/B, and HHV-7) DNA via multiplex PCR. Quantitative PCR was then performed only for CMV following first positive sample. CMV/HHV-6 co-infections were the most frequent co-infection, defined as the presence of DNA of ≥2 herpesviruses (HHVs) in the same sample, and patients with co-infection had more severe clinical outcomes (e.g. lymphopenia, rash, pneumonia, bacteremia, and fungal infections) compared to a single herpesvirus infection.
Patients who underwent hematopoietic stem cell transplantation (autologous or allogeneic) were excluded from this study and patients enrolled in this study did not receive any CMV antivirals (foscarnet, ganciclovir, or cidofovir). The mean age of the 95 patients was 16 (range 1-64 years). Of these 95 patients, 52 had acute lymphoblastic leukemia (ALL) and 43 had acute myeloid leukemia (AML). Seventy patients out of 95 achieved remission after induction therapy, while 15 had primary refractory disease and 10 died (8 AML and 2 ALL) in aplasia. Fifty-four of these 70 patients were in continuous complete remission after post-remission therapy, 14 relapsed and 2 AML patients died. Twenty-nine patients with relapsed or refractory acute leukemia were treated with salvage regimens. Eighteen of 29 patients achieved complete remission following salvage therapy, whereas 6 patients were refractory and 5 ALL patients died at the end of the study. Overall, 734 plasma tests were evaluated (median 7 samples per patient, range 3-20): 95 (from 95 patients) before chemotherapy, 247 (from 95 patients) post-induction, 257 (from 70 patients) post-remission, and 135 (from 29 patients) post-salvage.

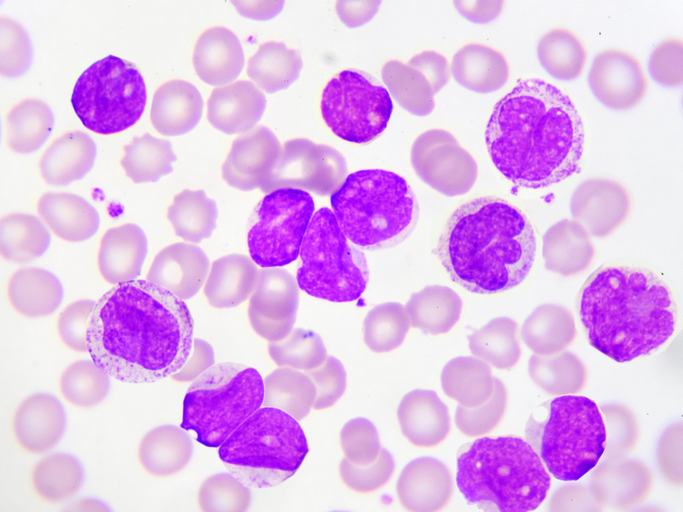
Single infections and co-infections in acute leukemia patients. Source: Virology Journal, 2020
In these 95 patients, IgG seroprevalence before chemotherapy was high (around 95%) for all the herpesviruses, with the exception of VZV (84.2%) and EBV (81%), indicating previous exposure to these ubiquitous herpesviruses prior to chemotherapy. Of the 95 patients, 60 had at one positive result for ≥1 of the HHVs analyzed; 33 (34.7%) patients had only one herpesvirus detected in any sample whereas 27 (28.4%) developed co-infection with ≥2 HHVs (21 had two viruses detected in any one sample and 6 had three viruses in any one sample).
Among all patients, CMV (48.4%) was the most frequently identified, followed by HHV-6 (26.3%), HHV-7 (14.7%), and EBV (8.4%). A majority (65.5%) of CMV reactivations were low-level reactivations (57.1-1,000 copies/mL) whereas 34.5% had high level reactivation (>1,000 copies/mL). Three persistent HHV-6 infections occurred in two patients. One patient had a first episode at post-remission followed by a second episode at salvage chemo; the other patient had two recurrent infections: one at diagnosis, then one at induction, followed by another one at post-remission. Fifteen patients (15.8%) were infected with CMV and HHV-6: 5 tested for HHV-6 first, 3 tested for CMV first, and 7 tested for both simultaneously. CMV DNAemia occurred more often at salvage therapy vs. before chemo or post-induction (p<0.05). HHV-6 was detected in 1% of patients before chemo, 3.15% at post-induction, 2.8% at post-remission, and 7% after salvage therapy. In this study, about 3/4 of HHV-6 infections were followed by a CMV infection, a phenomenon that has been reported in both solid organ (Phan 2018) and hematopoietic stem cell transplant recipients (Zerr 2005). HHV-6 was an independent risk factor for CMV infection (OR 4.205, p=0.008). Salvage treatment (OR 2.887, p=0.04) and CMV infection (OR 4.264, p=0.007) were independent risk factors for HHV-6 infection.
Overall, these investigators demonstrated that HHV reactivation occurs routinely in acute leukemia patients not immunocompromised by a transplant. CMV/HHV-6 was the most common co-infection. The clinical outcomes were worse in those with co-infection compared to single infection and suggest that these HHVs contribute to post-chemo morbidity.
Read the full paper here: Handous 2020